Current trends in anemia treatment in kidney transplant recipients
Ieva Ziedina1,2, Anete Granovska1, Viktorija Kuzema1,2, Aivars Petersons1,2.
1Department of Internal Diseases, Riga Stradins University, Riga, Latvia; 2Nephrology Center, Pauls Stradins Clinical University Hospital, Riga, Latvia
Background and Aims: The topic of management of chronic kidney disease (CKD) anemia has constantly been improving. This study aimed to assess the prevalence and current trends in anemia treatment in real-world kidney transplant recipients (KTR).
Methods: This cross-section study included 509 KTR patients, mean age – of 53 years, 51.5% male, with functioning grafts in the late post-transplant period in the last quarter of 2021, in an average of 9,4 years post-transplantation. Data were analyzed using SPSS Statistics 27.0. Student's t-test, Chi-squared test, Pearson correlation tests were used. According to the Kidney Disease: Improving Global Outcomes (KDIGO) definition, anemia was determined as a hemoglobin (Hb) level of <120 g/L for women and <130 g/L for men. CKD stage was determined by the estimated glomerular filtration rate (eGFR) calculated using creatinine in the CKD-EPI equation.
Results: The prevalence of anemia in the KTR population was 35% (n=178), increasing from 13% to 96% by progressing CKD from stage 1 to 5 in a transplant (Table 1: The prevalence of anemia depends on the stage of CKD in a transplant.) 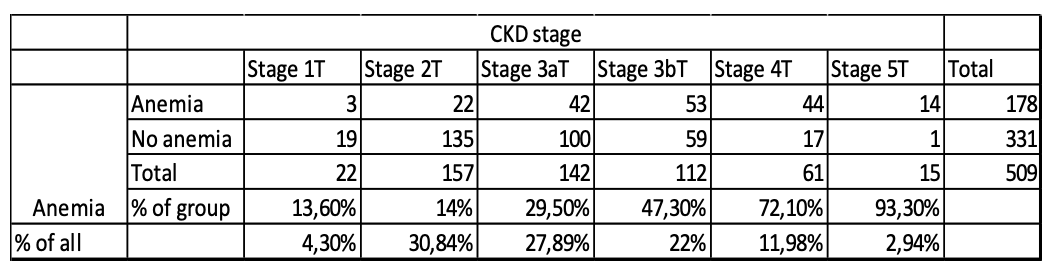 A moderately strong Pearson correlation was recognized between the stage of CKD and anemia (r=0.441; p<0.001). A statistically significant association (p<0.001) was detected between anemia and the female gender (n=107; 60% of all anemic patients). We found no significant association between anemia and the use of mycophenolate or calcineurin inhibitors. Still, there was a statistically significant association between steroid use and anemia (p=0.041), with a 31% (Odds Ratio = 0.69) less chance of anemia in a group that received steroid therapy. 90% of anemic patients had normochromic, normocytic anemia, 7,8% hypochromic, microcytic, and 2,2% hyperchromic, macrocytic anemia. The treatment involved iron replacement in 29% (n=51) of patients, of whom 92.2% had oral medication and 7.8% intravenous. 54% (n=96) of anemic KTR received treatment with erythropoiesis-stimulating agents (ESAs): 27,1% with darbepoetin alfa and 72,9% with methoxy polyethylene glycol-epoetin beta. Anemia was corrected up to Hb level >110 g/L in 69.7% (n=67) of ESAs receiving KTR. A statistically significant correlation was not detected between the ESAs dosage (µg/kg) and the correction of the anemia (p=0.217).
A moderately strong Pearson correlation was recognized between the stage of CKD and anemia (r=0.441; p<0.001). A statistically significant association (p<0.001) was detected between anemia and the female gender (n=107; 60% of all anemic patients). We found no significant association between anemia and the use of mycophenolate or calcineurin inhibitors. Still, there was a statistically significant association between steroid use and anemia (p=0.041), with a 31% (Odds Ratio = 0.69) less chance of anemia in a group that received steroid therapy. 90% of anemic patients had normochromic, normocytic anemia, 7,8% hypochromic, microcytic, and 2,2% hyperchromic, macrocytic anemia. The treatment involved iron replacement in 29% (n=51) of patients, of whom 92.2% had oral medication and 7.8% intravenous. 54% (n=96) of anemic KTR received treatment with erythropoiesis-stimulating agents (ESAs): 27,1% with darbepoetin alfa and 72,9% with methoxy polyethylene glycol-epoetin beta. Anemia was corrected up to Hb level >110 g/L in 69.7% (n=67) of ESAs receiving KTR. A statistically significant correlation was not detected between the ESAs dosage (µg/kg) and the correction of the anemia (p=0.217).
Conclusion: Like in the general CKD population, the prevalence of anemia in KTR increases as CKD progress in a transplant. The extent of anemia correction seems insufficient, although it includes both major components: iron replacement and ESAs. We found anemia more prevalent in female patients and those not receiving steroids in the immunosuppressive regimen. This last unexpected finding needs further exploration.
Darja Golubeva for data collection. Ieva Evelina Stolcere for data collection. Liana Linda Lice for data collection.

right-click to download
