The impact of a positive B-cell flow crossmatch in living donor renal transplant recipients
Jorge Chancay1, Luis Sanchez 1, Eileen Bogue1, Arjun Bhansali1, Fasika Tedla1, Manikkam Suthanthiran2, Prabhakar Putheti2, Ron Shapiro1, Graciela Deboccardo1.
1Recanati Miller Transplant Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Transplantation Institute, Weill Cornell School of Medicine, New York, NY, United States
Background: The aim of this study is to determine the incidence of early acute rejection and graft outcomes in living donor renal transplants with an isolated positive B-Cell Flow-Cytometry Crossmatch (B-FCXM).
Methods: We performed a retrospective analysis of graft outcomes in 152 adults who received living donor renal transplants between January 2019 and March 2021 at Mount Sinai Hospital in New York CIty. Pre-transplant histocompatibility was assessed with flow cytometric crossmatch (FCXM) and Luminex single-antigen beads. Positive B- FCXM is was defined as median channel shift of ≥ 40. A mean fluorescence intensity (MFI) ≥ 1400 defined positive donor-specific HLA Class I and/or II antibody (DSA). Most patients received induction immunosuppression consisting of rabbit anti-thymocyte globulin, steroids and intravenous immunoglobulin. Estimated glomerular filtration rate (eGFR) and biopsy-proven rejection at six months’ post-transplant were compared between patients with and without a positive B-FCXM, and positive and negative DSA.
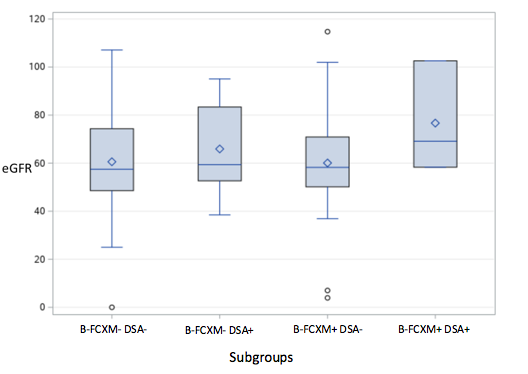
Results: Of 152 patients, 89 (59%) were males and 63 (41%) females; the mean age was 44 years (SD ± 13.8). 45 donor B-FCXMs (30%) were positive and 107 (70%) were negative. 42 (28%) positive donor B-FCXM had no DSA and 3 (2%) had DSA. 91 (85%) negative donor B-FCXMs did not have DSA, and 16 (15%) had DSA. Thirty-six (80%) out of 45 patients with positive donor B-FCXM, including the 3 patients with DSA, received intravenous-immunoglobulin (IVIG) as part of induction immunosuppression. None of the patients with both positive donor B-FCXM and DSA had rejection. eGFR and rejection rate at 6 months were similar between patients with positive and negative donor B-FCXM [median 58.9 (IQR= 50.2-70.8) vs 57.6 (48.8-76.6), p=0.88; 6.8% vs 5.6%, p=0.7, respectively]. Comparison by combination of donor B-FCXM and DSA status (B-FCXM- DSA-, B-FCXM- DSA+, B-FCXM+ DSA-, B-FCXM+ DSA+) did not show statistically significant differences in eGFR or rejection rate at 6 months [median 57.4 (IQR= 48.5-74.3) vs 59.3 (52.6-83.3) vs 58.2 (50.1-70.8) vs 76.6 (58.3-102.5) p=0.4; 3.3% vs 18.7% vs 7.3% vs 0% p=0.09, respectively].
Conclusion: In our cohort, there was no statistical difference in early acute rejection and graft function at 6 months between living donor transplant recipients with positive and negative donor B-FCXM even after accounting for DSA status. Peri-transplant treatment with IVIG for a positive donor B-FCXM might be a helpful adjunct in this setting.

right-click to download
