A single-center analysis of kidney transplant patients with COVID-19 compared to waitlisted in the two waves: an Indian report with future implications for the potential next wave
Hari Meshram1, Vivek Kute1, Himanshu Patel1, Sudeep Desai1, Subho Banerjee1, Akash Shah1.
1Nephrology and transplantation, IKDRC-ITS, Ahmedabad, India
Introduction: There is a paucity of data confronting the outcomes of COVID-19 in waitlisted compared to kidney transplant recipients from the developing world.
Methods: This was a retrospective cohort study of 334 hospitalized COVID-19 patients [waitlisted (n = 147) and KTR (n=187)] in a single center from India during two time periods of 5 May 20 to 23 September (first wave) and 26 March to 6 June 2021(second wave). We aimed to compare the demographic, clinical profile, laboratory features, outcomes and risk factors.
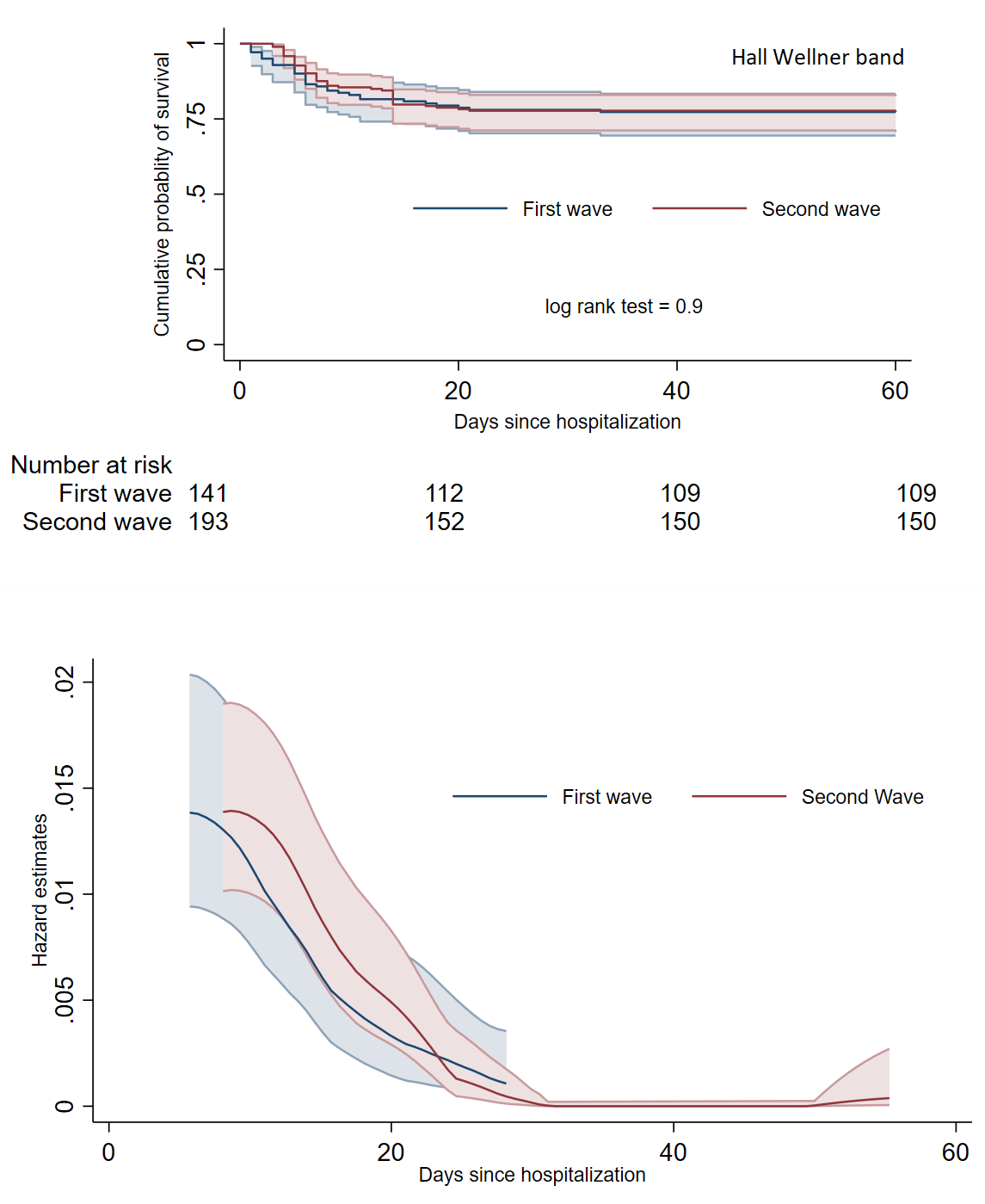
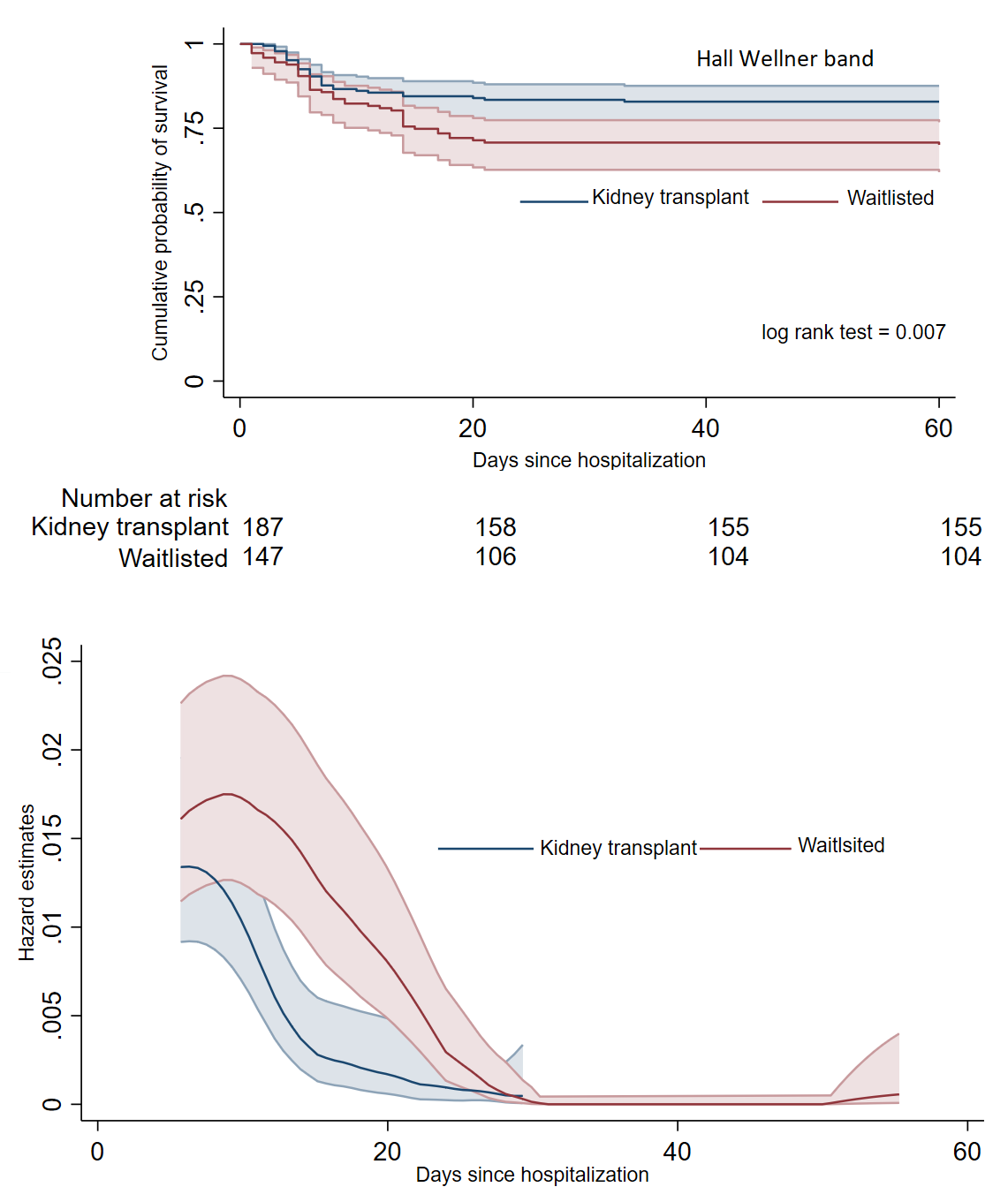
Results: Among the demographic characteristics, waitlisted group had older age [45(35-54) vs 40(32-48); p-value < 0.01] and equal gender distribution (56.4% vs 81.8%; p-value < 0.01) compared to kidney transplant recipients. Overall, waitlisted patients were more symptomatic. The unadjusted 60-day mortality remained same across both the pandemic waves (log rank test, p-value = 0.9) but was higher for waitlisted patients (30.6% vs 17%; log rank test, p-value = 0.007). In a univariable analysis age more than 60 years, waitlist status, hypertension, diabetes, obesity was associated significant mortality. In a multivariate analysis, age (OR = 5.7(2.3-14); p-value < 0.01), hypertension (OR = 11(4.1-28); p-value < 0.01) and diabetes (OR = 2.3(1.1-5); p-value = 0.02) was associated with mortality. In multivariate analysis for prediction of severe disease, only hypertensive cases (OR = 4.8(2.2-10.5; p-value < 0.01) was found having association.
Conclusion: Our report describes greater mortality in waitlisted patients which is mostly contributed to a higher burden of co-morbidities in this population.