
The use of mTOR inhibitors is associated with reduced mortality among kidney transplant patients developing COVID-19
Lúcio Requião-Moura1,2,6, Luís Gustavo Modelli de Andrade3,6, Tainá V Sandes-Freitas4,5,6, Marina P Cristelli2, Laila A Viana2, Mônica R Nakamura2, Valter D Garcia6, Roberto C Manfro6, Denise R Simão6, Ricardo Augusto M Barros Almeida6, Gustavo F Ferreira6, Kellen Micheline A Henrique Costa6, Paula R Lima6, Alvaro Pacheco-Silva6, Ida Maria M Fernandes Charpiot6, Luciane M Deboni6, Teresa Cristina A Ferreira6, Marilda Mazzali6, Carlos Alberto C Calazans6, Reinaldo B Oriá6, Hélio Tedesco-Silva1,2,6, José Medina-Pestana1,2,6.
1Nephrology Division, Universidade Federal de São Paulo, São Paulo, Brazil; 2Hospital do Rim, Fundação Oswaldo Ramos, São Paulo, Brazil; 3Department of Internal Medicine, Universidade Estadual Paulista-UNESP, Botucatu, Brazil; 4Programa de Pós-Graduação em Ciências Médicas, Universidade Federal do Ceará, Fortaleza, Brazil; 5Hospital Universitário Walter Cantídio, Universidade Federal do Ceará, Fortaleza, Brazil; 6COVID-19-KT Brazil Study Group, COVID-19-KT Brazil Study Group, Brazil
COVID-19-KT Brazil Study Group.
Background: The chronic use of immunosuppressive drugs is a key risk factor of death due to COVID-19 in kidney transplant recipients (KTRs), although no evident association between the class of immunosuppressive and outcomes has been observed. Thus, we aimed to compare COVID-19-associated outcomes among KTRs receiving three different immunosuppressive maintenance regime.
Methods: This study included data from 1,833 KTRs with COVID-19 diagnosed between Mar/20 and Apr/21 extracted from the national registry prior to immunization. All patients were taking calcineurin inhibitor (CNi) associated with mycophenolate (MPA, n=1,258), azathioprine (AZA, n=389) or mTOR inhibitors (mTORi, n=186). Outcomes within 30 and 90 days were assessed. Patient survival was estimated by Kaplan-Meier and the multivariable analysis was provided by center-adjusted Cox regression models.
Results: The overall hospitalization rate was 65.5% and was lower among patients in the CNi-AZA group compared with CNi-MPA (45.6% vs. 66.7%, p<0.001) and CNi-mTORi (45.6% vs. 61.1%, p=0.001, figure 3). The overall admission rate to the ICU was 32.3%, higher in the CNi-MPA than CNi-AZA (35.7% vs. 25.8%, p<0.001) and CNi-mTORi (35.7% vs. 22.6%, p<0.001). Last, 23.5% of the patients required mechanical ventilation, a higher proportion in the CNi-MPA group compared with CNi-AZA (26.8% vs. 17.8%, p<0.001) and to CNi-mTORi (26.8% vs. 13.4%, p<0.001). Compared with patients receiving MPA, the 30-day (79.9% vs. 87.9% vs. 89.2%, p<0.0001) and 90-day (75% vs. 83.5% vs. 88.2%, p<0.0001) unadjusted patient survival was higher in those receiving AZA or mTORi, respectively.
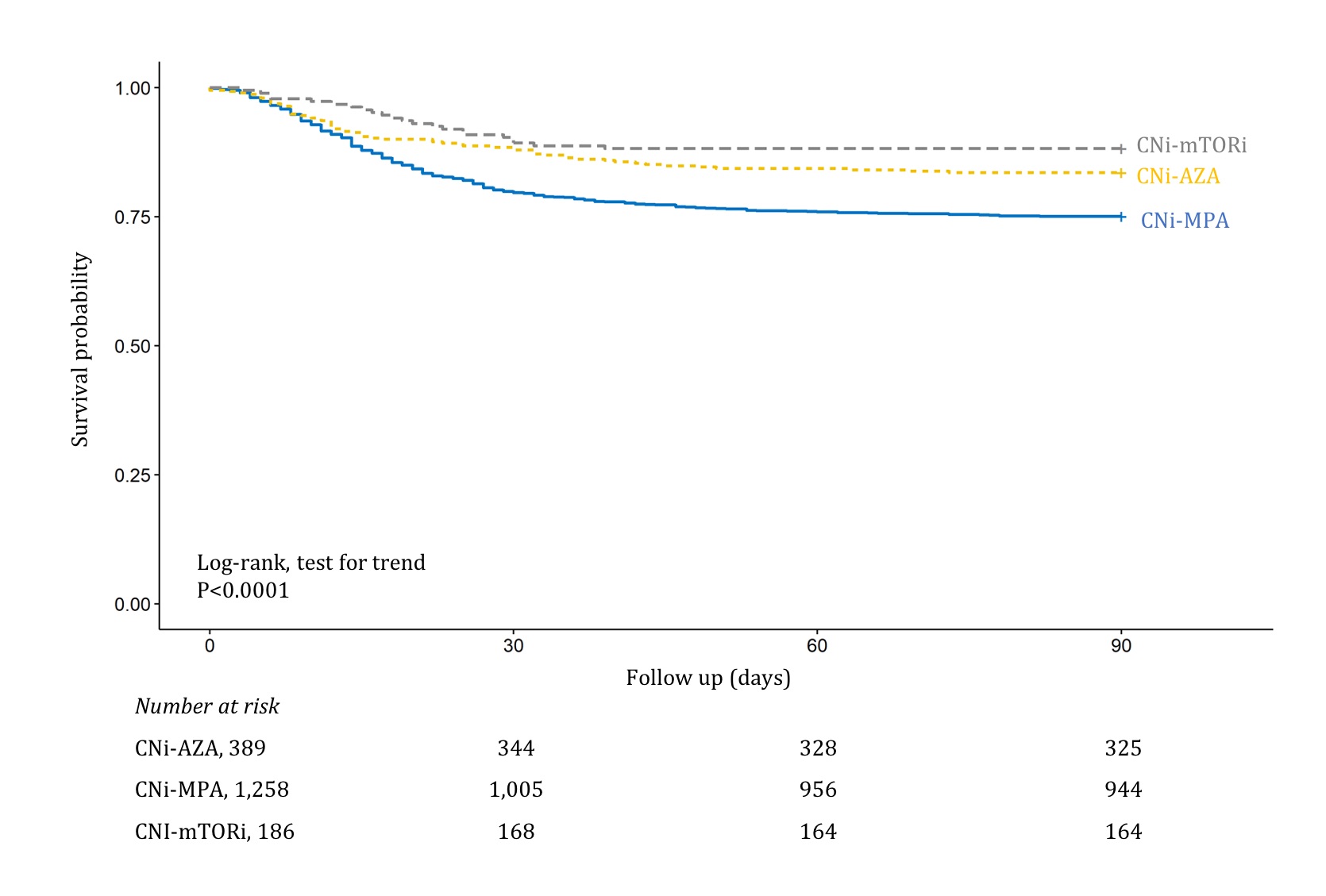
Using adjusted multivariable Cox regression, compared with patients receiving AZA, the use of MPA was associated with a higher risk of death within 30 days (aHR=1.70; 95%CI= 1.21–2.40; p=0.003), which was not observed in patients using mTORi (aHR=0.78; 95%CI= 0.45-1.35; p=0.365). At 90 days, while higher risk of death was confirmed in patients receiving MPA (aHR=1.46; 95%CI= 1.09-1.98; p=0.013), a reduced risk was observed in patients receiving mTORi (aHR= 0.59; 95%CI= 0.35-0.97; p=0.04) compared with AZA.
Conclusion: This national cohort data suggest that in kidney transplant recipients receiving CNi and diagnosed with COVID-19, the use of MPA was associated with higher while mTORi use was associated with lower risk of death.
