
Magnetic resonance imaging of renal oxygen metabolism by means of 17-O administration during ex vivo organ perfusion
Carolina Campos Pamplona1, Johannes J Castelein2, Tim TL Hamelink1, Veerle V Lantinga1, Baran B Ogurlu1, Jan Hendrik JH Potze2, Christian C Schuch3, Michael M Bock4, Henri HGD Leuvenink1, Ronald RJH Borra2, Cyril C Moers1.
1Surgery - Organ Donation and Transplantation, University Medical Center Groningen, Groningen, Netherlands; 2Radiology, University Medical Center Groningen, Groningen, Netherlands; 3NUKEM Isotopes GmbH, Alzenau, Germany; 4Radiology, University Medical Center Freiburg, Freiburg, Germany
Department of Surgery – Organ Donation and Transplantation, University Medical Center Groningen. Department of Radiology, University Medical Center Groningen. Department of Radiology, University Medical Center Freiburg.
Background: Renal normothermic machine perfusion (NMP) is a method studied for pre-transplant evaluation of kidney graft quality. This technique creates an isolated near-physiological environment by circulating a perfusion solution at body temperature with oxygen and nutrients. However, reliable ex vivo organ viability markers are still lacking. Magnetic resonance imaging (MRI) has recently been applied as a new rapid non-invasive technique to study renal viability ex vivo. Oxygen-17 (17O) offers a novel sensitive assessment of oxidative metabolism. In our MRI compatible perfusion setup, we aimed to study oxygen metabolism during NMP.
Methods: Three viable porcine kidneys were retrieved at a slaughterhouse and preserved by oxygenated hypothermic machine perfusion. In addition, one discarded human kidney was shipped to our center in static cold storage. Subsequently each kidney was perfused for 4 hours at 37°C inside a clinical 3T MRI scanner. Blood gas, glucose, and electrolytes were periodically monitored. Anatomical T2-weighted images and T2* maps were obtained using a 1H 18Ch-bodyflex coil and dynamic radial 17O MR images were acquired using a 17O Tx/Rx loop coil and a 17O 3D-UTE sequence. The 17O perfusion protocol consisted of 4 minutes of deoxygenation with nitrogen gas, 8 minutes of 70%-enriched 17O2 gas infusion at 0.1L/min, and 20 minutes of subsequent carbogen (95% O2 / 5% CO2) oxygenation. 17O-magnitude data was analyzed dynamically over time. To study the 17O-related global signal change, a region of interest was defined in the anatomical T2-weighted images and co-registered to the dynamic 17O-magnitude data.
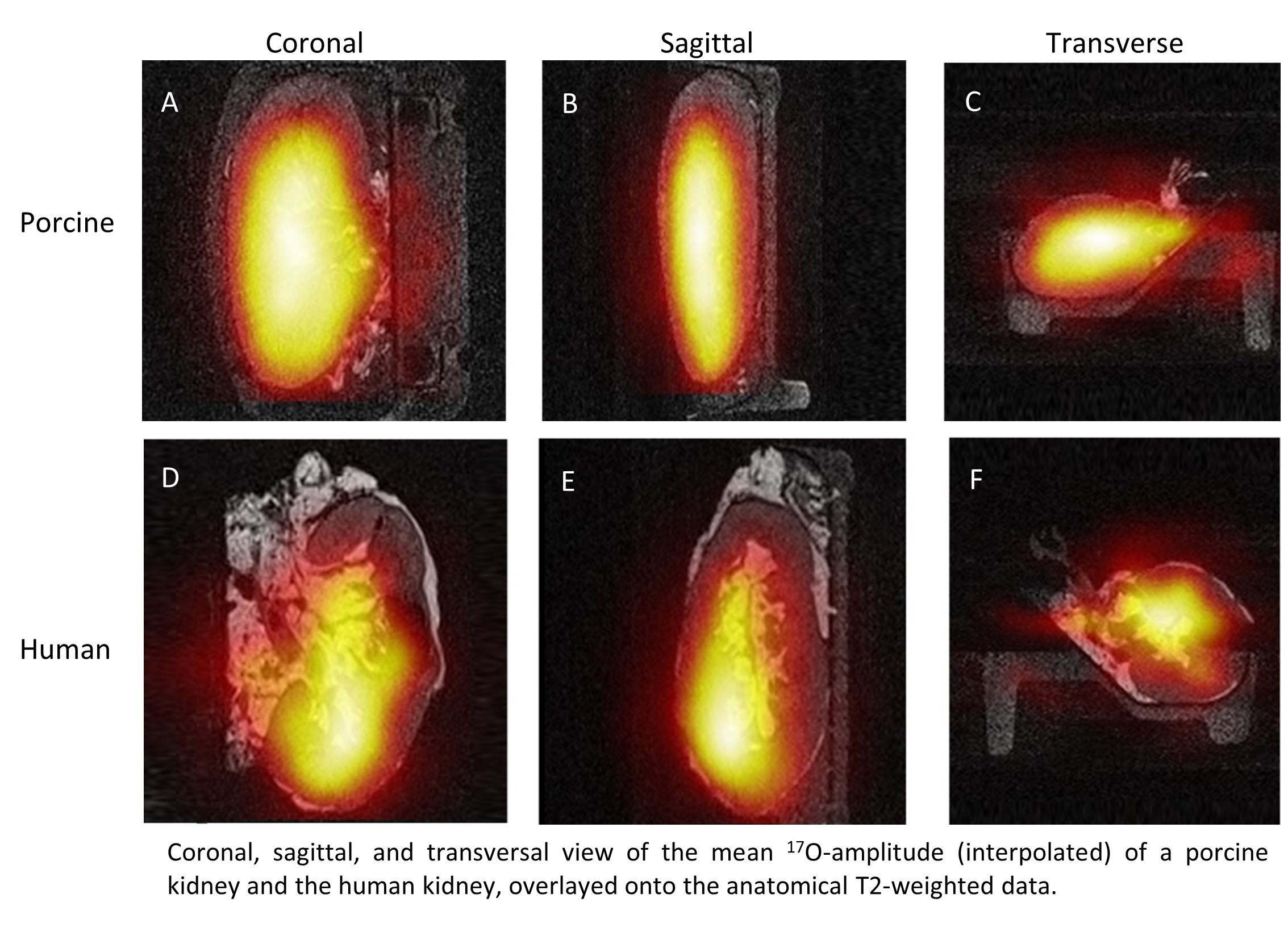
Results: Porcine kidneys showed homogenous perfusion with increased H217O-concentration in the medulla and decreased concentration in the cortex. The discarded human kidney demonstrated a focused concentration in the medial side of the lower pole with little to no signal intensity in the upper pole and the majority of the cortex, which was consistent with its reason for discard (wide cist in the lateral pole).
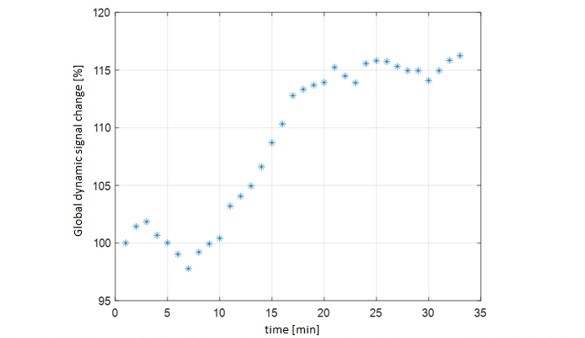
Six minutes after administration of 17O2-gas, a rapid H217O signal increase was observed until minute 20 of the dynamic acquisition, where saturation was reached and the signal plateaued. Overall, an enhancement of 16% between the first and last data point was measured.
Conclusion: In these pilot experiments, we were able to quantify the regional production of H217O in time, both in porcine and human kidneys. The slope of occurrence of H217O may be an interesting ex vivo organ viability biomarker, immediately related to the rate of oxidative metabolism in the organ and hence organ quality. As the kidney is in an ex vivo setting, any increase in H217O-concentration must be the direct result of metabolism within the organ. The current setup has great potential for investigating renal oxygen metabolism ex vivo.
NUKEM Isotopes GmbH, Alzenau, Germany. Department of Radiology, University Medical Center Freiburg, Freiburg, Germany.
