Donation after cardiac death (DCD) liver grafts from elderly donors: a comparative analysis of feasibility and outcome
Samrat Ray1, Catherine Parmentier1, Markus Selzner1, Ian McGilvray1, Blayne Sayed1, Chaya Ganor Shwaartz1, Mark Cattral1, Anand Ghanekar1, Gonzalo Sapisochin1, Cynthia Tsien1, Nazia Selzner1, Leslie Lilly1, Mamatha Bhat1, Trevor Reichman1.
1Ajmera Transplant Centre, Toronto general hospital, Toronto, ON, Canada
Introduction: Advanced donor age is a known factor to affect the post-operative functional outcome of deceased donor liver transplantation (DDLT) and is in fact the biggest attributable factor to high donor risk index (DRI). When paired with donation after cardiac death (DCD), the risk of transplantation increases several folds thereby precluding the use of such grafts at most centres worldwide. With a high threshold of rejecting such grafts at our centre, we aim to analyse the outcomes of liver transplantation using elderly DCD grafts and assess its feasibility.
Methods: All patients having undergone DDLT between January 2016 and December 2021 were included in the study. The population was divided into 4 groups: DCD grafts (<50 years and >50 years) and DBD (Donation after brain death) grafts (<50 years and >50 years). The peri-operative and post-operative outcomes were compared. The borderline grafts having placed on Organox machine perfusion for optimisation were excluded from the study (n=38).
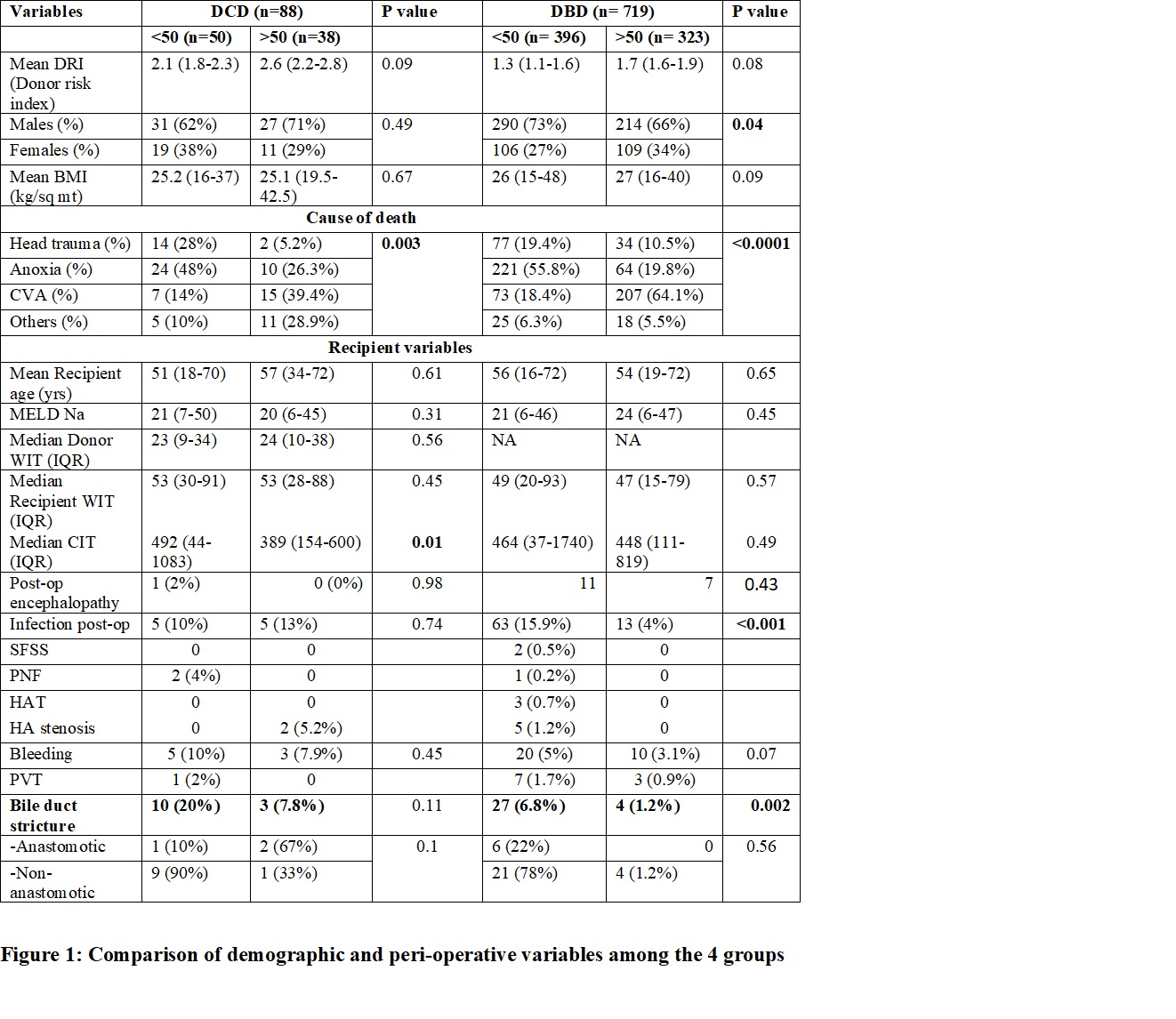
Results: Of the 807 patients included in the analysis, 88 (10.9%) received a graft from the DCD donors including MAiD (Medically assistance in dying) donors, with 38 (43%) of them being from the elderly donors. In the DBD group (n=719; 89%), 323 (45%) received grafts from the elderly donors. The demographic and peri-operative parameters were comparable in both groups (Figure 1).
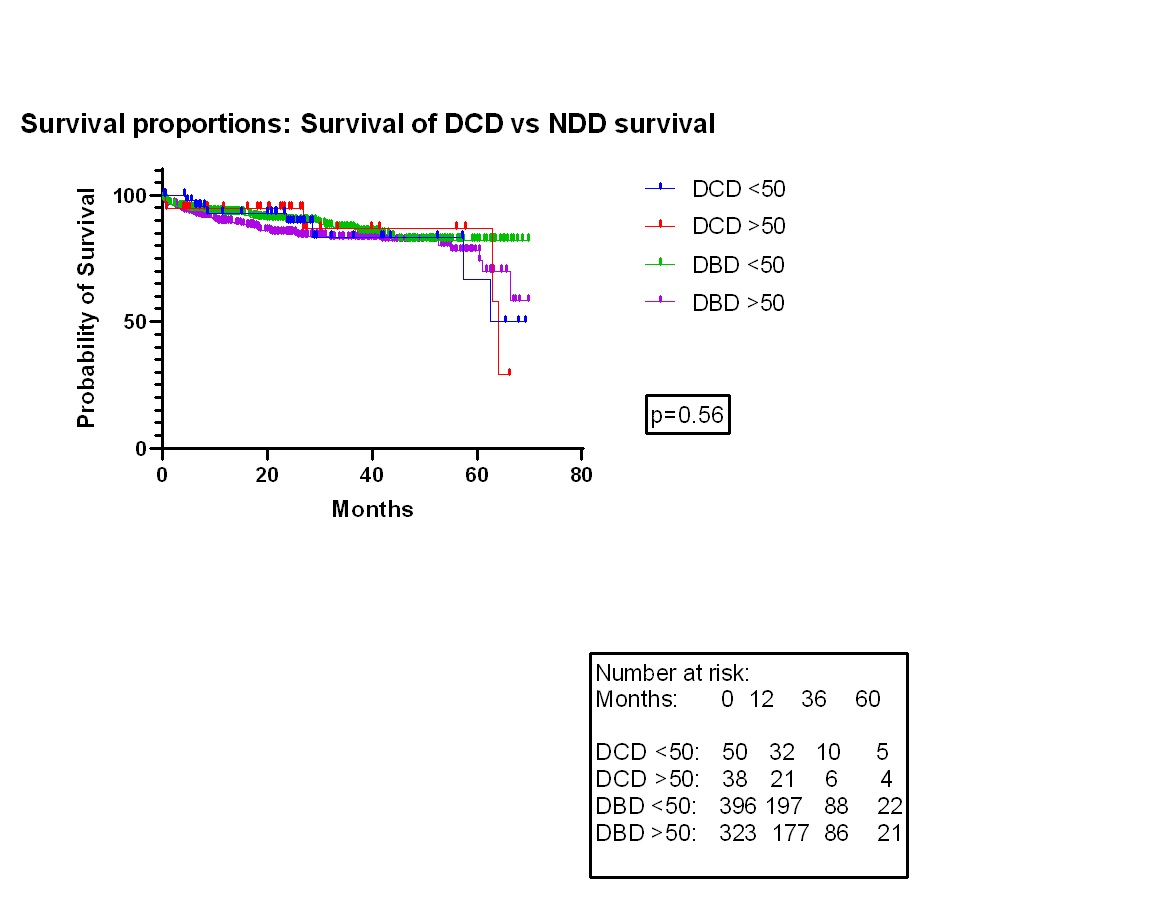
The overall incidence of post-operative biliary stricture was higher for the DCD grafts compared to DBD (13; 14.7% vs 31; 4.3%; p=0.001). However, the same was slightly lower in the elderly DCD group (n=3; 7.8%) compared to the younger group (n=10; 20%); p=0.11, with a higher occurrence of anastomotic stricture in the elderly group (n=2; 67%) and non-anastomotic in the younger group (n=9; 90%); p=0.1 (Figure 1). There was no significant difference between the mortality of the younger vs elderly groups in DCD (14% vs 13%; p=0.9) and DBD (10% vs 6%; p=0.06) cohorts. The 1-,3- and 5- year survival of the DCD grafts (94%, 88%, 62%) were comparable to that of the DBD grafts (95%, 87%, 72%); p=0.09. Also, the patients receiving elderly DCD grafts showed similar graft survival rates compared to the younger DCD grafts (90%, 80%, 68% vs 91%, 81%, 65%; p=0.56). There was no significant difference in the 1-,3-and 5- year survival rates of patients among the 4 groups (Figure 2).
Conclusion: Donor age alone should not be the criteria to decide the acceptability of DCD grafts in liver transplantation. With proper selection criteria, elderly DCD grafts could be a valuable contributor to expand the liver donor pool with comparable results to lesser damaged younger DBD grafts.
