Ngee-Soon S Lau, Australia has been granted the TTS-TSANZ International Transplantation Science Mentee-Mentor Awards

Factors determining the ex-vivo survival of human livers more than 1 week under normothermic conditions: understanding the requirements for long-term survival of organs
Ngee-Soon Lau1,2,3, Mark Ly1,2,3, Claude Dennis5, Joanna Lou Huang1,2,3, Joanna Huang1,2,3, Andrew Jacques1,2,3, Marti Cabanes-Creus2,4, Shamus Toomath1,2, Nicole Mestrovic1,2,3, Paul Yousif1,2, Sumon Chanda1,2, Chuanmin Wang1,2,3, Leszek Lisowski4, Ken Liu1,3, James Kench3,5, Geoffrey McCaughan1,2,3, Michael Crawford1,2, Carlo Pulitano1,2,3.
1Australian National Liver Transplantation Unit, Royal Prince Alfred Hospital, Sydney, Australia; 2Centre for Organ Assessment, Repair and Optimisation, Royal Prince Alfred Hospital, Sydney, Australia; 3Faculty of Medicine and Health, University of Sydney, Sydney, Australia; 4Children’s Medical Research Institute, The University of Sydney, Sydney, Australia; 5Department of Tissue Pathology and Diagnostic Oncology, Royal Prince Alfred Hospital, Sydney, Australia
Introduction: Current ex-vivo technology allows the perfusion of an organ only for a number of hours. There is a need for perfusion in the range of days-to-weeks to facilitate sophisticated assessment, recovery and modification of these organs. Normothermic perfusion of livers longer than 1 week has never been previously described. In this study, we aimed to develop a model which reliably maintained the physiological function of human livers for more than 1 week and understand the requirements of these organs for long-term survival.
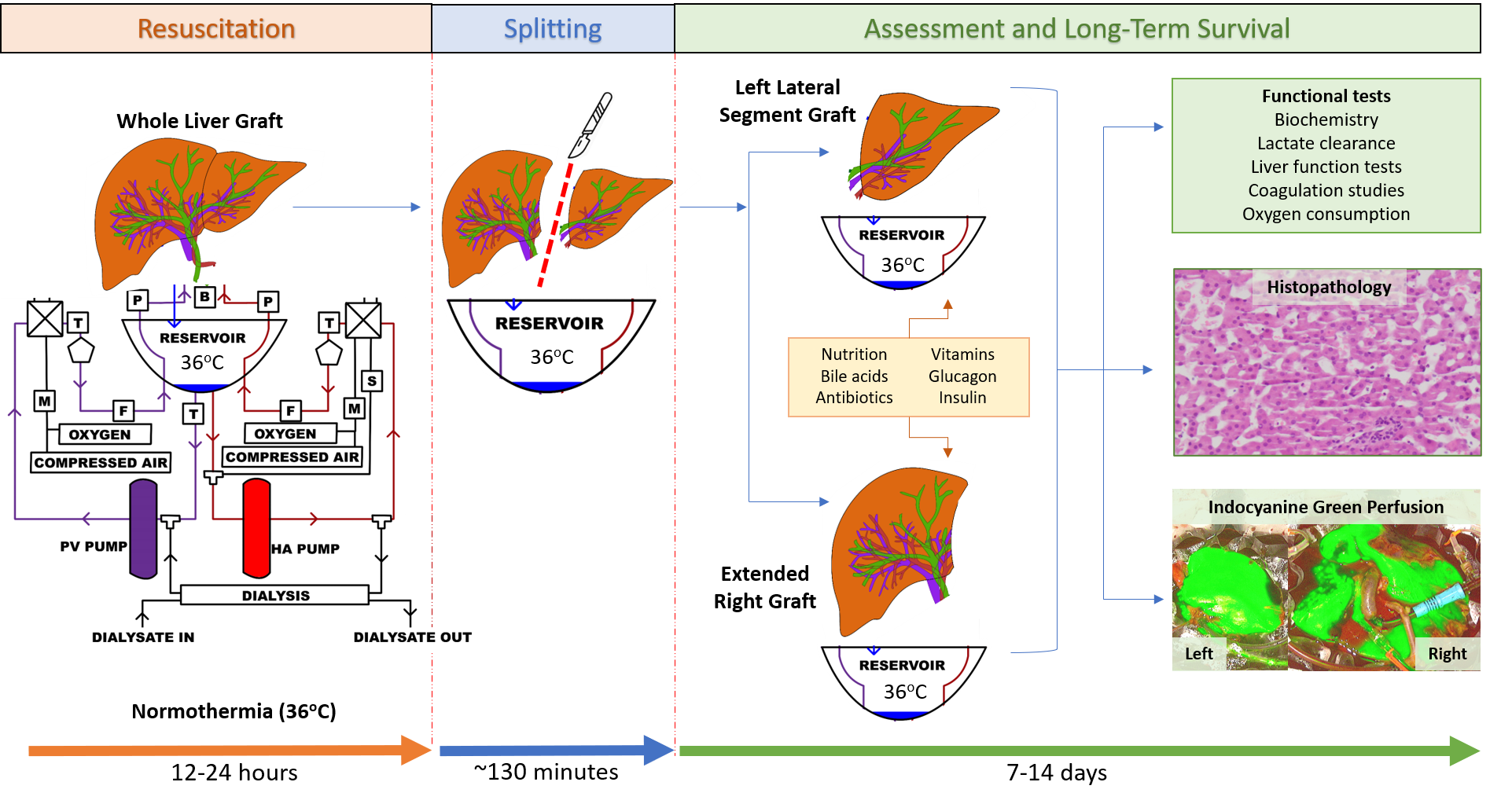
Method: We developed a protocol for long-term organ perfusion using a modified commercial system which included long-term oxygenators, a gas-mixer and a dialysis filter. Human livers not suitable for transplantation were perfused using a human red-cell based perfusate under normothermic conditions (36°C) and then surgically split without interruption to perfusion. The resulting left lateral segment grafts and extended right grafts were then perfused on separate machines for the purpose of long-term survival and individual graft assessment with biochemical and histological markers of liver function (Figure 1). Novel methods for understanding the cause of graft failure of these human livers in the long-term were used including indocyanine green perfusion, microbial cultures, lipidomics, metabolomics and assessment of pro-inflammatory cytokines.
Results: Ten livers underwent a conventional split during normothermic perfusion resulting in 20 partial grafts. The median ex-vivo survival was 165 hours, and the longest survival was 328 hours (13 days) (Figure 2). Graft survival was demonstrated by lactate clearance, bile production and production of Factor-V in the long-term. A total of 9/20 (45%) grafts survived for ≥7 days. These grafts demonstrated a significantly higher bile production adjusted to graft weight and a significantly higher level of perfusate Factor-V in the first 48 hours of perfusion (Figure 2). All grafts eventually failed with a predictable and repeatable pattern which include: increasing vascular resistance, unresponsive hypoglycaemia, acidosis and growth of mixed flora microbial contaminants.
Conclusion: We report a reliable and repeatable protocol for the long-term ex-vivo perfusion of human livers for more than 1 week. Possible reasons for organ failure during long-term perfusion include overwhelming infection and a failure to meet all long-term metabolic requirements. Future work should aim to overcome these barriers with the goal of preservation for weeks-to-months, if not indefinitely.