
Custom bone massive allograft for lower limb salvage surgery, the impact of imaging and 3D printing. Experience of the tissue bank of the hospital Luis Vernaza (2016-2021)
Winston Jaramillo1, Maria Ceballos1, Jorge Armijos2, Luis Moreira2, Diego Campoverde1.
1Banco de Tejidos, Hospital Luis Vernaza, Guayaquil, Ecuador; 2Traumatologia, Instituto Oncológico Nacional Dr. Juan Tanca Marengo, Guayaquil, Ecuador
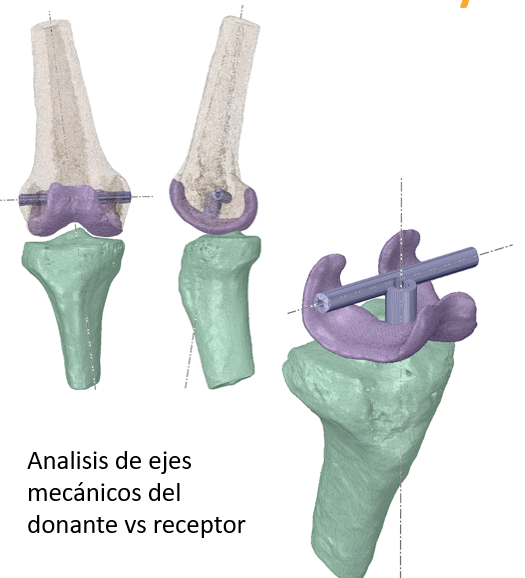
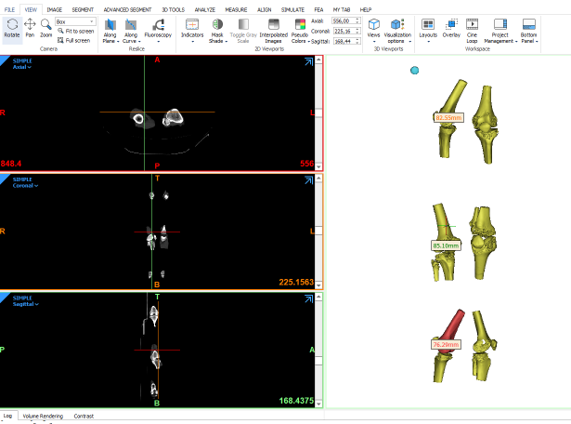
Introduction: Luis Vernaza Hospital tissue bank implemented the anatomical engineering service, which performs the activities of digitizing stored tissues, virtual surgical planning of custom tissues, and the generation of cutting guides for efficient osteotomies between donor and recipient. The main use of this technology is to provide allografts of the proximal tibia or distal femur for salvage surgery of the lower limb, with which it has been possible to restore the mobility and functionality of the knee to patients with bone tumors. With this technology, we have managed to deliver custom allografts with a discrepancy of 1 to 2 mm between the measurements of the recipient and that of the donor, in addition to obtaining three-dimensional measurements such as the curvature of the femoral condyle and the curvature of the femorotibial joint.
Objective: To present the results obtained by the anatomical engineering service in the development of custom fabrics for lower limb salvage surgery.
Materials and Methods: The complete knee joint, including 20 cm of the distal femur and 20 cm of the proximal tibia, is obtained from cadaveric donors. Then we proceed with the digitalization of the tissues using computed axial tomography, a service provided by the imaging center of the Luis Vernaza Hospital. At the time of requesting a graft, the specialist attaches the tomography of the recipient with the indications and measurements of the graft to be requested. The search for the graft is carried out with it in the digital catalog of the tissue bank and using the Mimics anatomical engineering software using segmentation in volumes, the approximate measurements between recipient donors are obtained. Analyzing the curvature of the femoral condyle and the surface of the tibial plateau. With the indicated stockings, we proceed with the processing of the tissue, extracting the required tissue and the ligamentous elements necessary for its subsequent fixation.
Results: Thanks to this technology, it has been possible to restore mobility to 10 patients aged between 15 and 56 years. The most frequent pathology was osteosarcoma (6) followed by giant cell tumor and metastasis from other sites. The most requested graft was the proximal tibia 6 requested units, distal femur 3 units, and 1 humerus. Approximately the amount of tissue replaced was 15 cm.
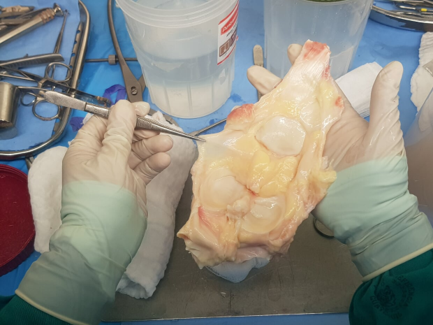
Discussions and Conclusions: It is difficult to obtain a synthetic replacement for the proximal tibia or distal femur, due to their multiple compositions (bone tissue, cartilage, and ligamentous fixing elements). Applying this technology to the tissue bank avoids the amputation of limbs due to lack of elements for reconstruction, because of which the allograft from a cadaveric donor with the exact stockings allows rapid restoration of the patient's mobility and return to their usual activities.
