Over 1,000 pancreas transplantation in a latin american program
Marcelo Perosa1, Juan Branez1, Fernanda Danziere1, Leonardo T. Mota1, Beimar Zeballos1, Marcio Paredes1, Aline R. Magalhães1, Leon Alvim1, Ana Claudia Vidigal1, Celia Watanabe1, Tércio Genzini1.
1Department of Abdominal Organ Transplantation, Leforte Hospital, São Paulo, Brazil
Introduction: There has been a worldwide tendency of decline in the annual number of pancreas transplants(PT). The maintenance of high-volume PT programs is of major importance both for assistance goals as for teaching of new generation of PT surgeons and clinicians. We aim to present the lessons learned from over 1,000 PT in a brazilian program.
Methods: We analyzed a 25-year period according to PT activity, immunosuppression, surgical techniques, postoperative management and outcomes.
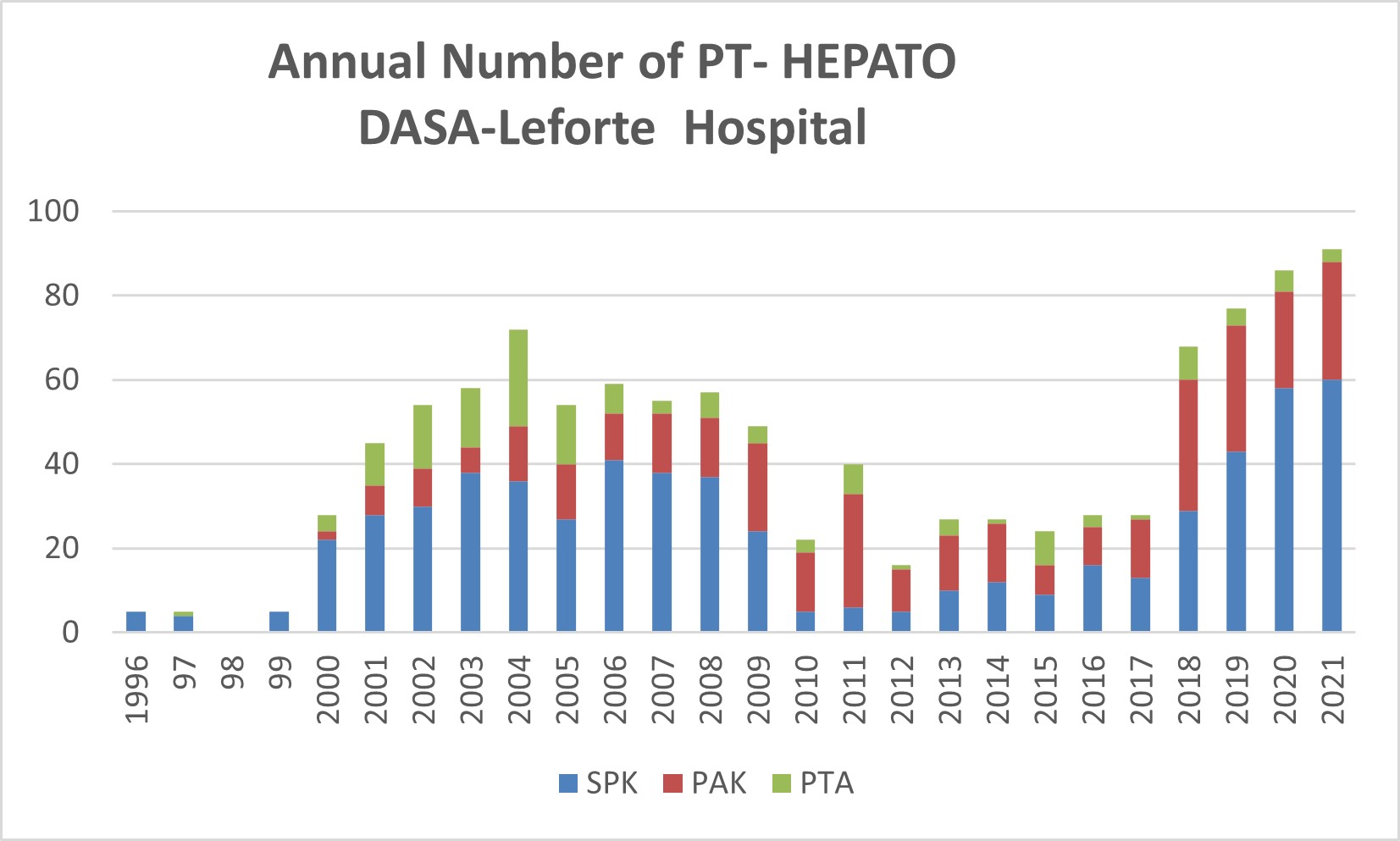
Results: Overall, 1,081 PT were analyzed, being 601 SPK and 480 solitary PT, out of which 331 PAK and 149 PTA. We have maintained a high-volume activity over these 25 years, highlighting the growing of the program in more recent years(Figure).Over half of our pancreas donor are procured outside of our regional and very frequently we procure donors in distant states of the country. Since 2014, pancreas allocation has been based on virtual crossmatch which has significantly reduced our mean ischemia time for approximately 8hours. In 2008 our program performed one third of the overall PT of the country and in 2020, 59% of overall national PT. As our mean waiting time for SPK has been about 2 years, we have encouraged patients to living-kidney donation, allowing living-kidney transplant first followed by PAK or simultaneous pancreas and living-donor kidney transplants. Our immunosuppression protocol has evolved from induction with OKT3 to a non-induction protocol in SPKs and then to depleting induction with thymoglobuline for all PT and maintenance with tacrolimus, mycophenolate mophetil or sodic and steroids. Surgical techniques were initially systemic-bladder, progressing to systemic-enteric(duodenojejunostomy), then portal-enteric, portal duodenal and more recently systemic(cava)-duodenal drainage. Postoperative management has also improved and based on early discharge(between 5-7 of days hospital stay) and a day-clinic basis follow-up, completing the remaining thymoglobulin or antibiotic doses as outpatient. In recent years a routine DSA monitoring has been performed and continuous CMV monitoring from post-transplant weeks 3 to 12 and preemptive treatment with valganciclovir when necessary. The rate of kidney DGF has been quite steady and roughly 40-50% due to limited conditions of donor maintenance in local hospitals. Our overall outcome has also evolved in most recent years achieving 1-year patient survival over 90% and pancreas and kidney survival over 80% with a reduction in technical failure to less than 10%.
Conclusion: Our PT program has been maintained as high-volume over the last decades and jumped to a very active(over 60 PT yearly) in the last 4 years. This growing was determined by evolution in different areas from donor and recipient selection to an optimized post-transplant management.