The genetic epidemiology of hereditary pancreatitis in Australia and its effect on patients of total pancreatectomy and islet auto translation (TP-IAT)
Denghao Wu1,2, Christopher Drogemuller1,2, Richard Couper1,2, David Torpy1,2, Hamish Scott1,3, Lyle Palmer1, Sunita De Sousa1,2,3, Patrick Toby Coates1,2.
1School of Medicine, University of Adelaide, Adelaide, Australia; 2Kidney and Islet Transplantation, Royal Adelaide Hospital, Adelaide, Australia; 3Centre for Cancer Biology, SA Pathology, Adelaide, Australia
Centre for Clinical and Experimental Transplantation.
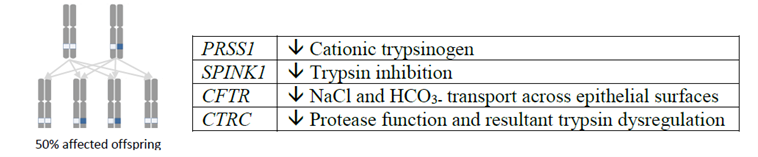
Introduction: Hereditary Pancreatitis (HP) is a cause of pancreatitis in childhood leading to lifelong disability and an elevated risk of pancreatic cancer. The clinical and genetic features of HP have not been characterised in Australia. This project aims to understand the effects of HP-associated variants on disease risk and progression, and their pertinence on past and future patients of TP-IAT.
Methods: HP patients were identified from existing hospital records. Interviews were administered to collect HP-associated data including pain management, medical prescriptions, interventions, smoking and alcohol history, and overall quality of life. Saliva samples were obtained for whole-exome-sequencing (WES). Genetic data were analysed using standard bioinformatics toolkits for variant discovery and correlation with HP phenotype. This was compared to a control sample of 2,504 patients with adult-onset chronic pancreatitis.
Results: A total of 44 HP patients from 10 independent pedigrees were identified. Eighty-four percent of HP cases presented with clinical onset before the age of 10. Eighty-six percent of HP patients reported ongoing opioid use to control pain and 79% of patients reported ongoing moderate to severe pain. The majority (57%) of the HP cohort self-identified as Indigenous Australians and HP was 67 times more prevalent in Indigenous populations than non-Indigenous. Overall, 14/16 individuals underwent TP-IAT exhibited substantial reduction in analgesic requirement. The estimated prevalence of HP in SA was 2.48 per 100,000. HP was ~67 times more prevalent in Indigenous people than non-Indigenous South Australians. The study cohort had a younger age of onset and higher female ratio when compared to 2,504 of control adult-onset CP cases.

Conclusion: Our estimated prevalence of HP is higher than previously described and disproportionately affect Indigenous populations. The percentage of HP patients requiring lifelong analgesics is alarming and genetic factors are an important cause of pancreatitis in Australian children. Finally, TP-IAT has been successful as a new therapy for HP management.
