Cat scratch related acute glomerulonephritis in a kidney transplant recipient
Anish Bhakta2, Swee-Ling Levea2, Laila Lakhani2, Lee Anderson2, David Wojciechowski2, Jose Torrealba1.
1Pathology, University of Texas Southwestern, Dallas, TX, United States; 2Nephrology, University of Texas Southwestern, Dallas, TX, United States
Objective: Bartonella Henselae (BH) infection is known to lead to life-threatening complications, especially amongst immunocompromised kidney transplant patients. We report a case of post-infectious glomerulonephritis in a kidney transplant recipient secondary to BH.
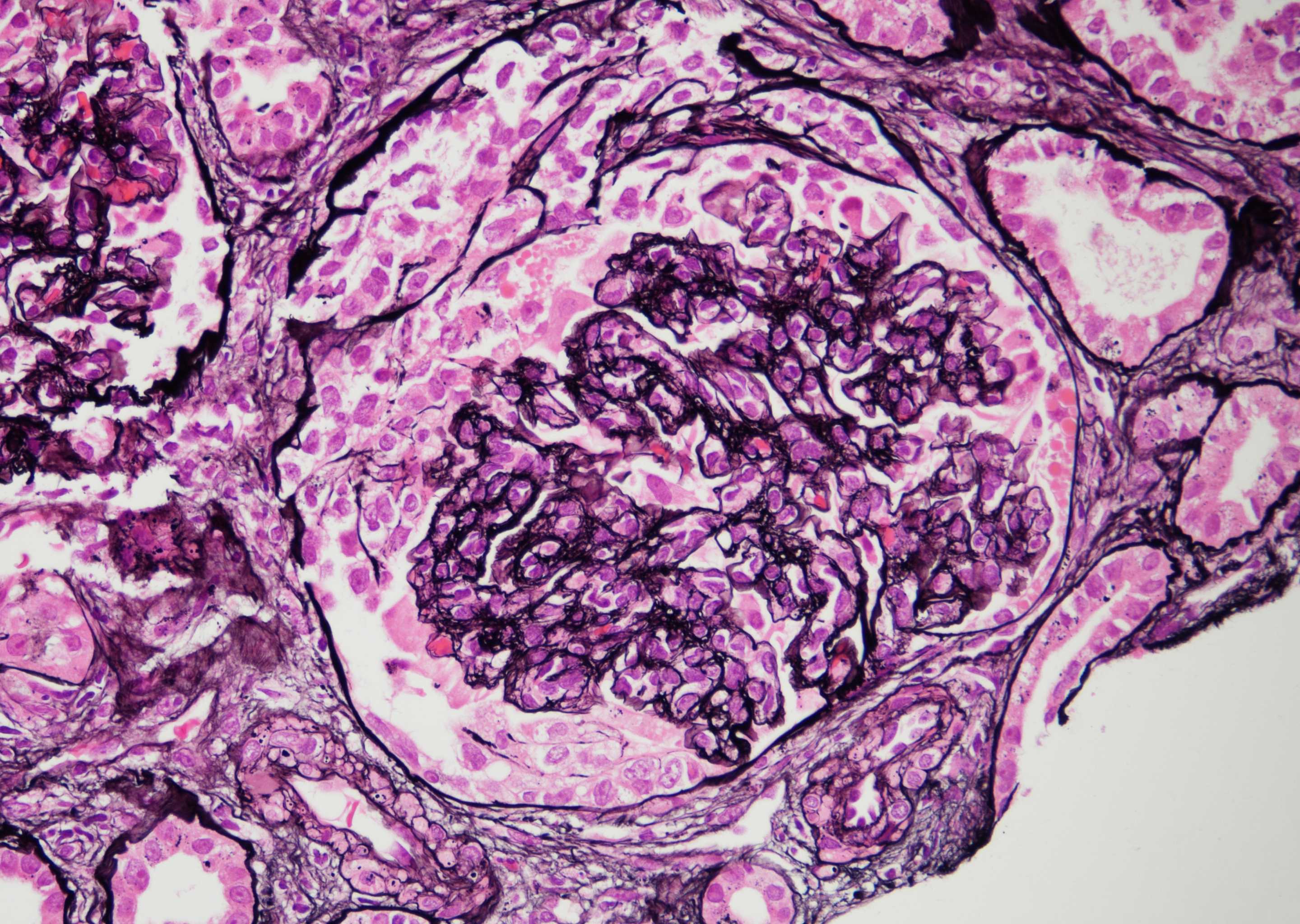
Methods: A 42-year old man who underwent a deceased donor kidney transplant with a baseline creatinine of 2 mg/dL, on tacrolimus and mycophenolate based immunosuppression regimen with early steroid withdrawal, presented 4 months post-transplant with AKI, fever and pancytopenia. Labs are as shown in Table 1.
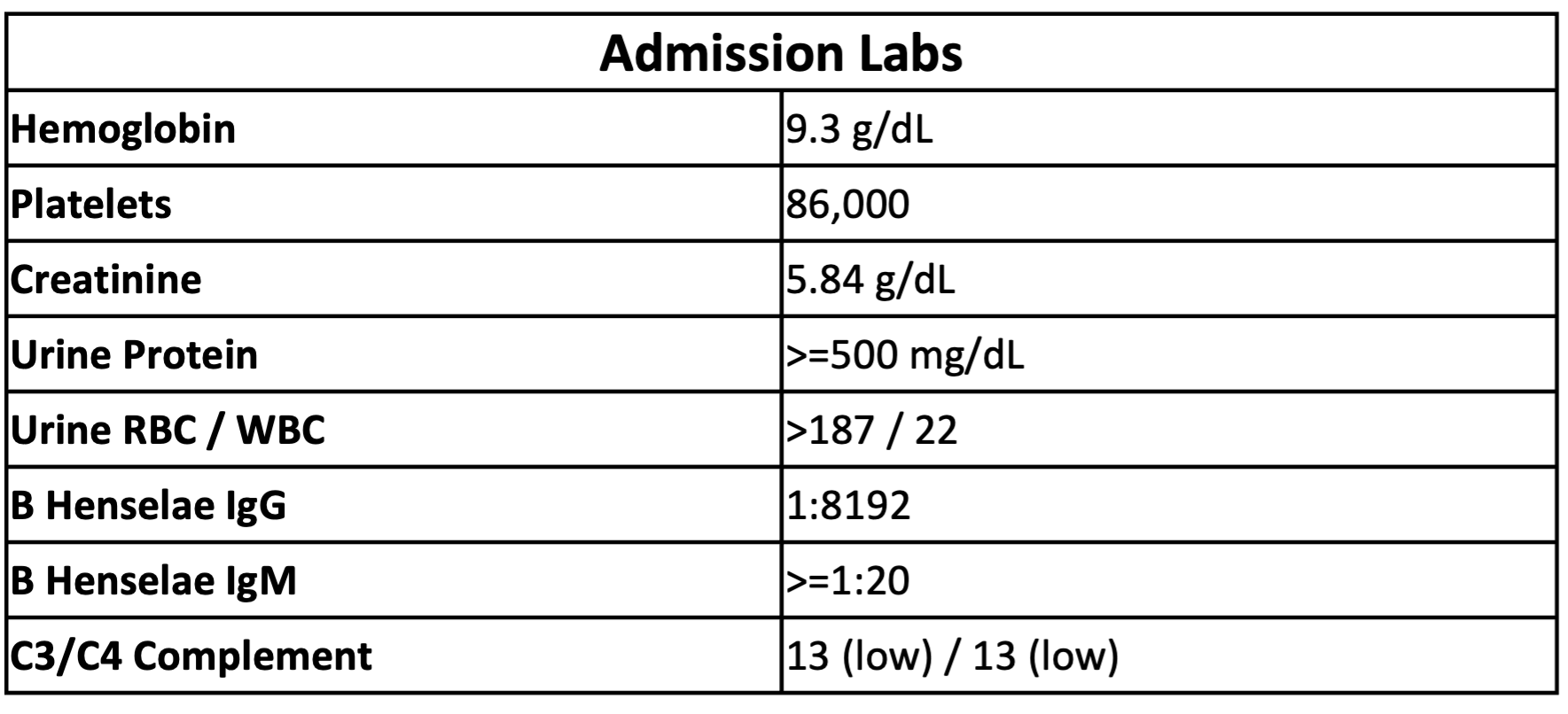
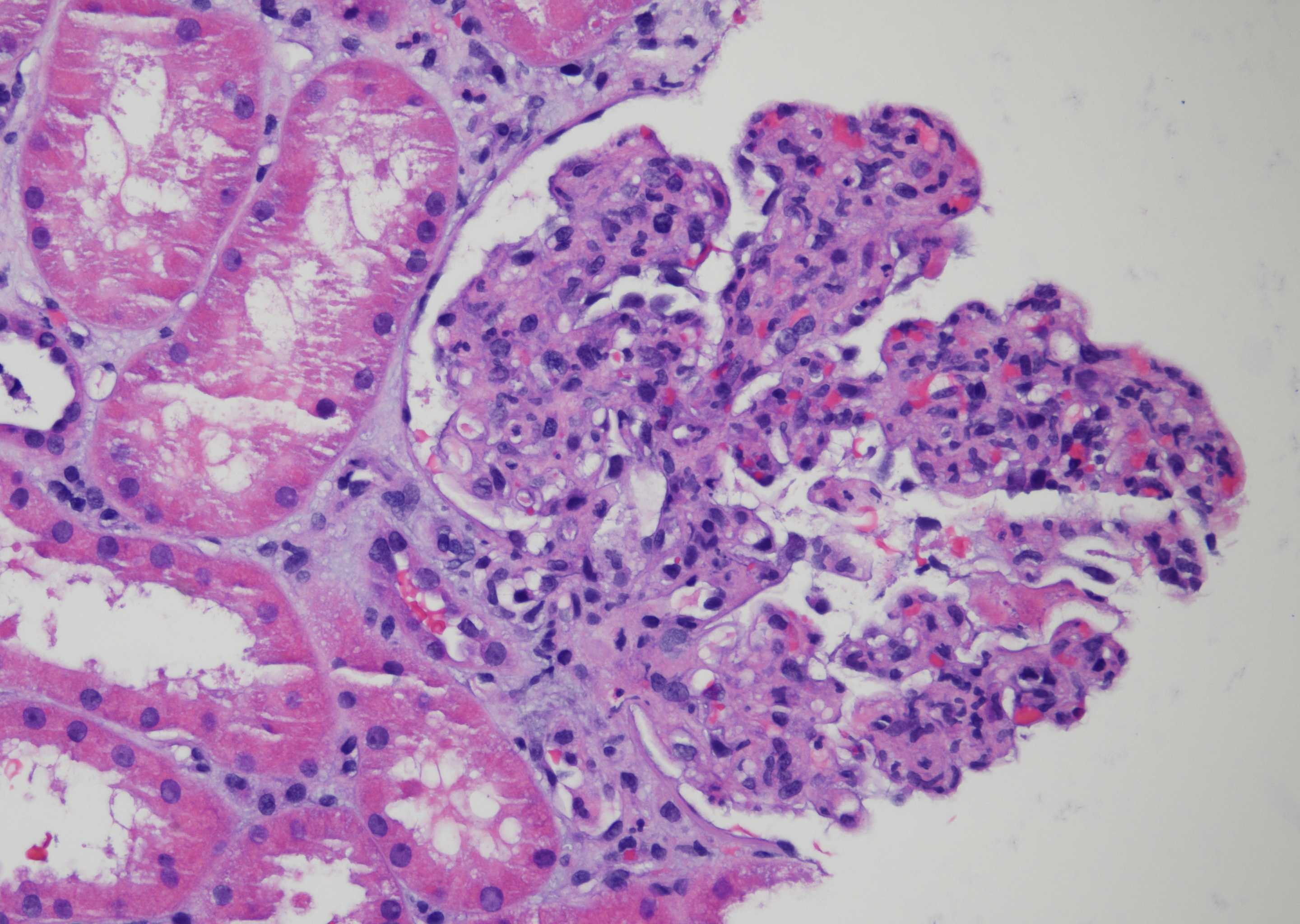
Results: Work up was notable for bartonella henselae bacteremia. He underwent an allograft biopsy that demonstrated post-infectious glomerulonephritis (GN); Mycophenolate was discontinued and treatment was started with rifabutin and doxycycline. AKI initially improved, but later worsened and a second biopsy was performed, which revealed a pattern of diffuse suppurative proliferative GN (Fig.1) with focal crescents (Fig. 2). Electron microscopy revealed sub-endothelial and sub-epithelial electrondense immune deposits. The immune deposits were predominantly IgA, IgM and C3, and negative for IgG. He was started on IV steroid pulse and initiated on dialysis for worsening volume overload. Four weeks after discharge a follow-up biopsy was performed as the patient remained on dialysis. The biopsy showed a focal proliferative GN with more segmental intra-membranous immune deposits and rare sub-epithelial humps, a pattern consistent with resolving post-infectious GN. Soon after he came off dialysis with resolving acute kidney injury.
Conclusions: There is limited literature published on infection related glomerulonephritis in transplant recipients with Bartonella. The few documented cases with Bartonella post-transplant have been seen in association with native valve endocarditis. Our patient had no vegetation on Echocardiogram. Given the severity of disease on pathology, with crescents, pulse dose steroids likely helped decrease inflammation. This is a unique case of Bartonella induced infection related glomerulonephritis that led to AKI requiring dialysis with resolution following treatment with antibiotics, immunosuppression reduction and steroid therapy.