Renal transplant outcomes: hepatitis C-infected donors and recipients
Hayley Cleveland1, Medhi Tavakol2, Satoshi Ashimine2, Christopher Freise2, Peter Chin-Hong1.
1Department of infectious Disease, University of California, San Francisco, San Francisco, CA, United States; 2Division of Transplant Surgery, Department of Surgery, University of California, San Francisco, San Franscisco, CA, United States
Background: There remains a shortage of kidneys available for transplantation. Increasing the utilization of hepatitis C virus infected organs could reduce the supply demand mismatch in organ transplantation. There is little data about long-term HCV renal transplantation outcomes in the era of effective direct-acting antivirals (DAA). It is important to determine precise outcomes of HCV-positive (HCV+) organs that are transplanted into HCV+ recipients (HCV D+/R+) to quantify risk for patients and other stakeholders, especially as HCV+ organ transplantation continues to expand to HCV-negative (HCV-) recipients.
Methods: We performed a retrospective cohort study of all cases of renal transplantation involving HCV+ recipients at a single academic medical center from 2008-2019. Data was extracted from the institutional electronic transplant database. Demographics, time to transplantation, incidence of organ rejection, and mortality data were compared between HCV D+/R+ and HCV D-/R+ groups.
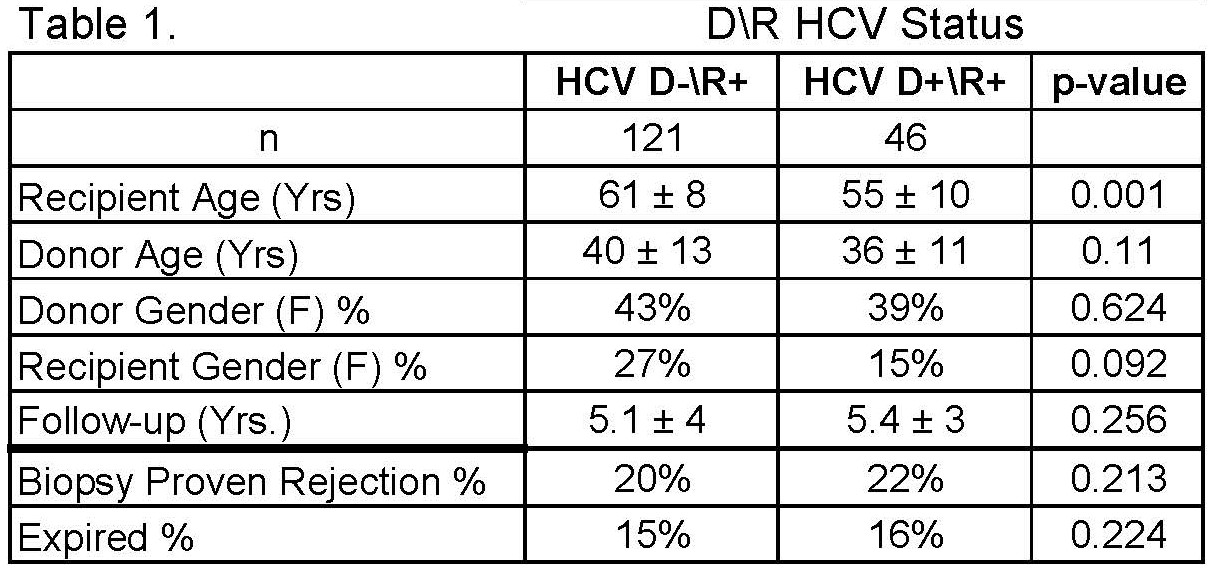
Results: We performed a retrospective study of 3781 kidney transplant recipients between 2008 and 2019. Patients were divided according to recipient/donor CMV serology status at the time of transplant. 121 were HCV D-\R+ and 46 were HCV D+\R+. Table 1 shows recipient and donor demographics stratified by D/R HCV serology status. Both groups had similar donor mean age and gender distribution. There were slightly more men and older recipients among HCV D+\R+ compared to the HCV D-\R+ group. The follow-up years were similar between both groups. The time to transplant for those who consented to receive an HCV+ kidney from the time of signing the consent was 407 days vs. 1210 days for those who did not consent. (p=0.0001). The incidence of rejection and mortality were similar between two groups at follow up. In Cox Hazards Model, we found no association between HCV D+/R+ and increasing risk of rejection or mortality (HR=0.79, 95% CI 0.36-1.74, p>0.20 and HR=0.99, 95% Cl 0.41-2.4, p>0.20,respectively: Figure 1.). Using a multivariate analysis, we found recipient age as the only independent risk factor for mortality (HR =1.08, 95% CI 1.01-1.14, p=0.015).
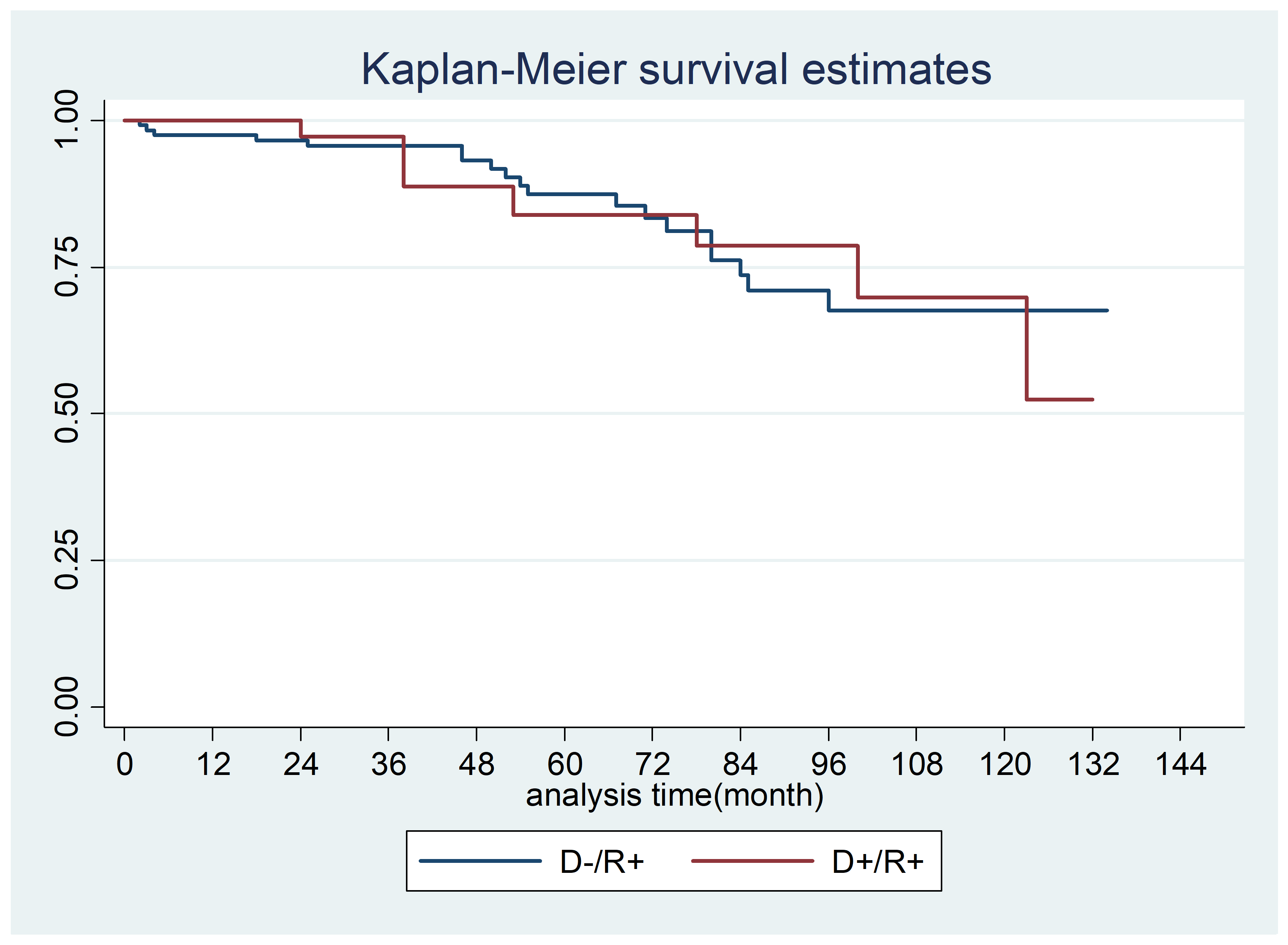
Conclusion: In analyzing 10 years of data at a single center, HCV+ renal transplant recipients did not have worse rejection or mortality if they received HCV+ kidneys compared to HCV- kidneys. Time to transplant was significantly decreased for those who consented to receive an HCV+ kidney as compared to those who did not. This data can be used to counsel HCV+ patients about accepting an HCV+ kidney for transplant, perhaps even encouraging it. Increasing the utilization of HCV+ kidneys for transplantation in the era of effective DAA has the potential to offer life-saving treatment to substantially more patients, along with decreasing time to transplantation.
