Transplant of the abdominal rectus fascia in rodents, first report of the microsurgical procedure, and initial results
Jeremías Moreira1, Pablo Stringa3, Virginia Gentilini1, Constanza Arriola1, Pablo Farinelli2, Martín Rumbo3, Gabriel Gondolesi2.
11- Instituto de Medicina Traslacional, Trasplante y Bioingeniería; Universidad Favaloro-CONICET, Capital Federal, Argentina; 22- Servicio de Cirugía General, Trasplante hepático, Pancreático e Intestinal, Hospital Universitario Fundación Favaloro, Capital Federal, Argentina; 33- Instituto de Inmunología y Fisiopatología, Universidad Nacional de La Plata (IIFP-UNLP-CONICET), La Plata, Argentina
Introduction: After intestinal or multivisceral transplants, the proper management and closure of the abdominal wall becomes a challenge. The enterocutaneous fistulas, ostomies, skin scars secondary to multiple previous surgeries or frozen abdomen syndrome are some of the predisposing factors. Synthetic meshes usually produce complications associated with infections and fistulas when used in unfavorable environments, in addition to high costs. Some previous clinical studies have shown benefits applying wall reconstruction techniques including the variant of using a non-vascularized fascia of the abdominal rectus muscle, described by our team. The need to better understand immunological aspects of this procedure we have conceived the concept of performing a murine model.
Methods: The procedures were approved by the internal review board and ethics committee for the care and use of laboratory animals (CICUAL UF 2021-016, #PICT 2016-3677). Technical aspects were done reproducing the technique for humans, details and pitfalls are described as part of the results. Engraftment observations were made on days 7, 11, and 30 post-transplantation for each animal strain. At day 30, each recipient was sacrificed, serum and tissue samples were obtained (from the sheath, and the adjacent muscle tissue). Histological studies of the graft were performed.
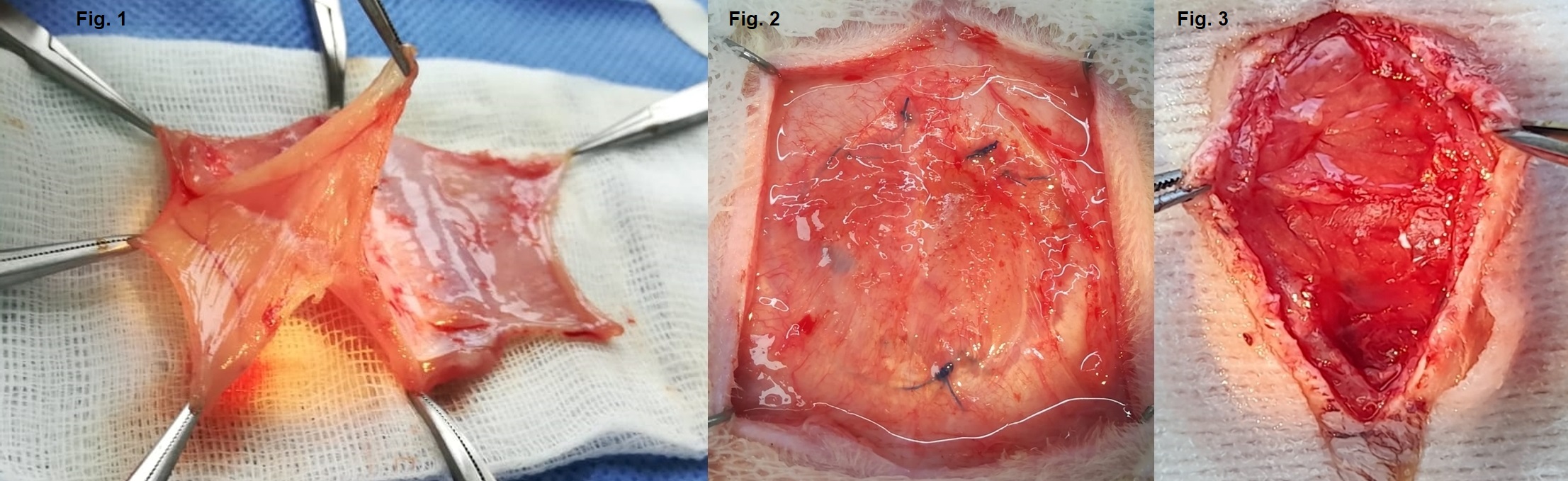
Results: 6 transplants of the abdominal rectus fascia (TxARF) were performed. All donors were female Sprague Dawley rats, while the recipients were 3 Sprague Dawley (3 isogenic TxARF) and 3 Wistar females (allogeneic TxARF). The skin was separated, and the abdominal muscle wall was completely removed to then perform the dissection under a microscope (Fig. 1). TxARF was done utilizing a continuous suture kind Surget with 6-0 Prolene, after removing the ARF and muscle of the recipient (Fig. 2), the skin is closed over the fascia. Once the Tx was finish a strict clinical follow-up of each rat was carried out providing initial treatment with Tramadol and Ceftriaxone; 30th day survival was 100%, 2 recipients developed seromas on days 5 and 11, both isogenic ARF. The visual observation of the grafts showed absence of tissue stiffness and the presence of macroscopic neovascularization (Fig. 3) None of the grafts presented visceral adhesions at the end of the observation period. On histological inspection, the grafts showed, no presence of leukocytes or apoptosic cells, the adjacent native muscle tissue did not present particularities.
Conclusion: This first report of the TxARF in rodents, proofs the feasibility of these experimental and translational model. Likewise, it shows similar results to the published in the clinical field, there was absence rejection and abdominal adhesions in the short term under a model without immunosuppression. Further studies will be done to evaluate the immunogenicity, the loss of strength and elasticity as well as the long term results of transplanting the ARF.