Mortality on the waiting list for pediatric patients requiring liver containing intestinal grafts in Argentina, how can we reverse the lack of donors?
Gabriel Gondolesi1, Vanina Tagliafichi2, Pablo Glitz2, Maria Florencia Fernandez1, Veronica Busoni3, Diego Ramisch1, Rodrigo Sanchez-Claria3, Liliana Bisigniano2.
1HPB and complex gastrointestinal surgery and abdominal organ transplant, Hospital Universitario Fundacion Favaloro, Caba, Argentina; 2Dirección Cientifico Técnica, INCUCAI, Caba, Argentina; 3Hospital Italiano, Caba, Argentina
Introduction: Pediatric patients requiring liver containing intestinal grafts have higher mortality on the waiting list compared to isolated intestinal transplant or pediatric liver transplant candidates. Major reasons being lack of young pediatric brain death donors (BDD). We aim to analyzed the mortality on the waiting list for pediatric recipients waiting for liver containing intestinal grafts.
Material and Methods: Retrospective analysis of all pediatric patients listed for combined liver+intestine or MTV, grouped as liver containing intestinal candidates (pLvCITx), and compared to pediatric isolated intestinal transplant (pIITx) and cadaveric liver transplants (pLTx) between 2006 and 2022. Variables including: age, sex, time on the waiting list, mortality, drop-out or rehabilitation while in the waiting list, were analyzed. Number of pediatric BDD was analyzed by periods (2006-2013 (P1) and 2014-2021 (P2), and age group). SPSS v20.0 was used for statistical analysis.
Results: A total of 33 pLvCITx were included in the analyses and compared to 84 pIITx and 1162 pLTx (table 1). The total number of pLvCITx in P1 was 8 and in P2 3, the number of IITX was 26 and 10 respectevily; and the number patients who died on each list were: 5 and 6 for the pLvCITx; 4 and 4 for the pIITx (p=N/S). The number of drop outs by periods for pLvCITx was: 5 and 1; while them were 10 and 3 for the pIITx group.
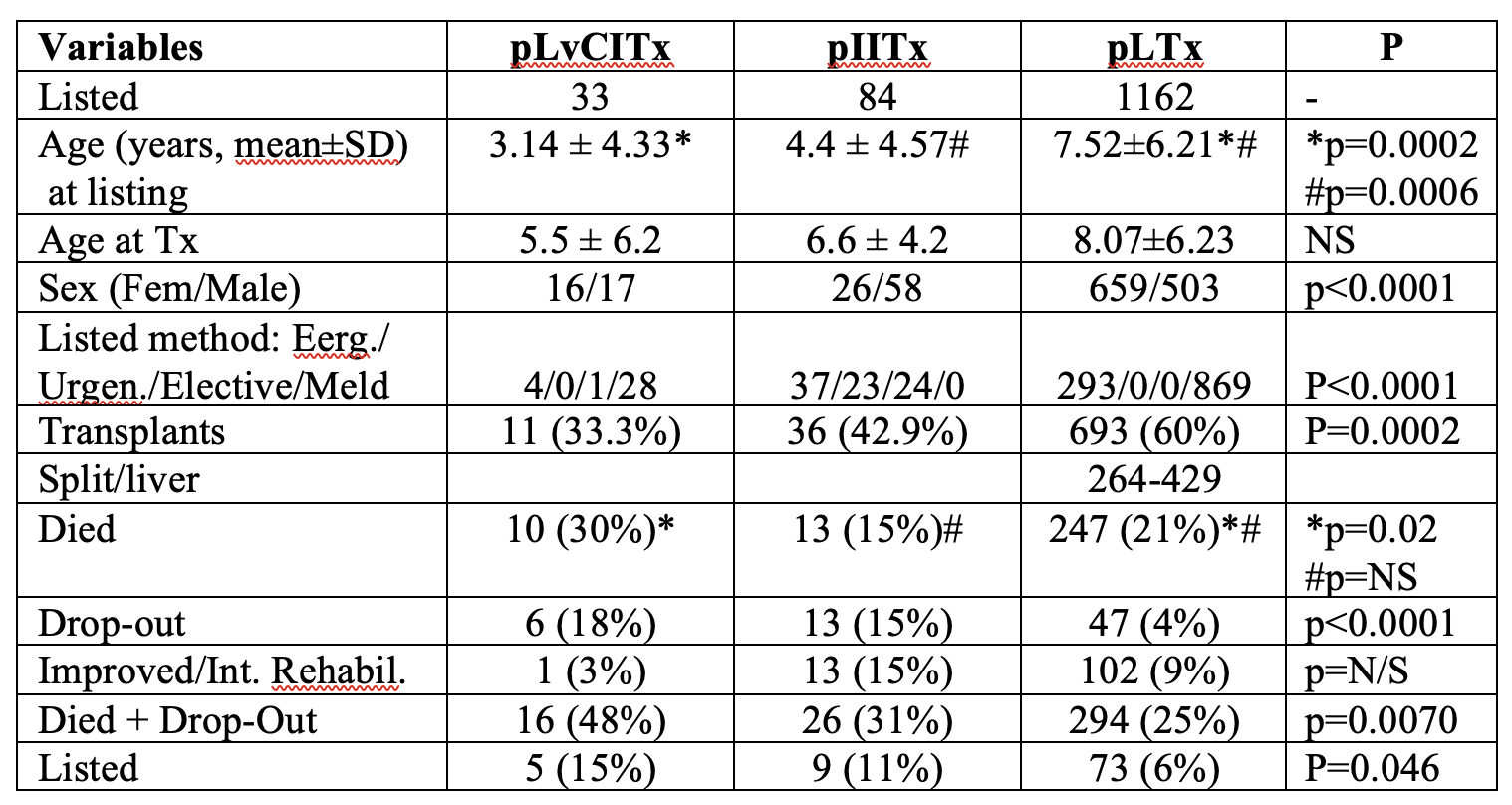
There were 714 pediatric BDD, 207 youngers than 10 years, and from them only 24 had less than 1 year; but 21 existed in P1, and only 3 in P2 (p=0.0035); similarly, for those between 1 and 5 years, there were 83, 51 in P1, and 32 in P2 (p=N/S). If deaths and drop-out are combined in the analysis, 48,5% of the pLcCITX, and 31% are at risk, vs 25% for the pLTx (p=0,007). A higher number of pIITx are able to improve while listed compared with the pLcCITx or pLTx. The 3-year KM survival on the waiting list for pLvCITx was 52%, being 81% for pIITx, and 64% for pLTx (log rank: p=0.04).
Conclusions: Mortality in the waiting list remains higher for pediatric patients waiting for a pCLvITX; although pIITx candidates had a higher drop-out while listed, that group has higher chances of improving or of being transplanted; and although donation remains low, it has become critical, and worsening in the last 7years for recipients below the year of age.
