Successful pregnancy in a small bowel syndrome patient without any nutritional support. Case report: GLP-2 levels in pregnancy and breastfeeding
Maria Virginia Gentilini1,2, Adriana A Crivelli Dr1, Mariana M Doeyo Dr1, Luis L Perez Illidge Dr1, Mariana Ortega1, Constanza C Arriola PhD1,2, Martín M Rumbo Prof3, Héctor H Solar Dr1, Gabriel Eduardo G Gondolesi Prof. Dr. 1,2.
1Multiorgan Transplant Institute, Nutritional Support Unit, Intestinal Rehabilitation and Transplanta, Favaloro University Hospital, Caba, Argentina; 2Translational Research Laboratory and Immunology associated to Transplantation, IMETTyB- CONICET, Favaloro University , Caba, Argentina; 3Immunology and Pathophysiology Studies Institute, (IPSI-CONICET) School of Exact Sciences, National , La Plata, Argentina
Introduction: Pregnant patients with Short Bowel Syndrome (SBS) and chronic intestinal failure (CIF) can successfully reach to term their pregnancies while on Parenteral Nutrition (PN) but with high rates of complications. The availability of entero-hormones, especially semisynthetic glucagon like peptide 2 (sGLP2) has increased the chances to achieve intestinal sufficiency.
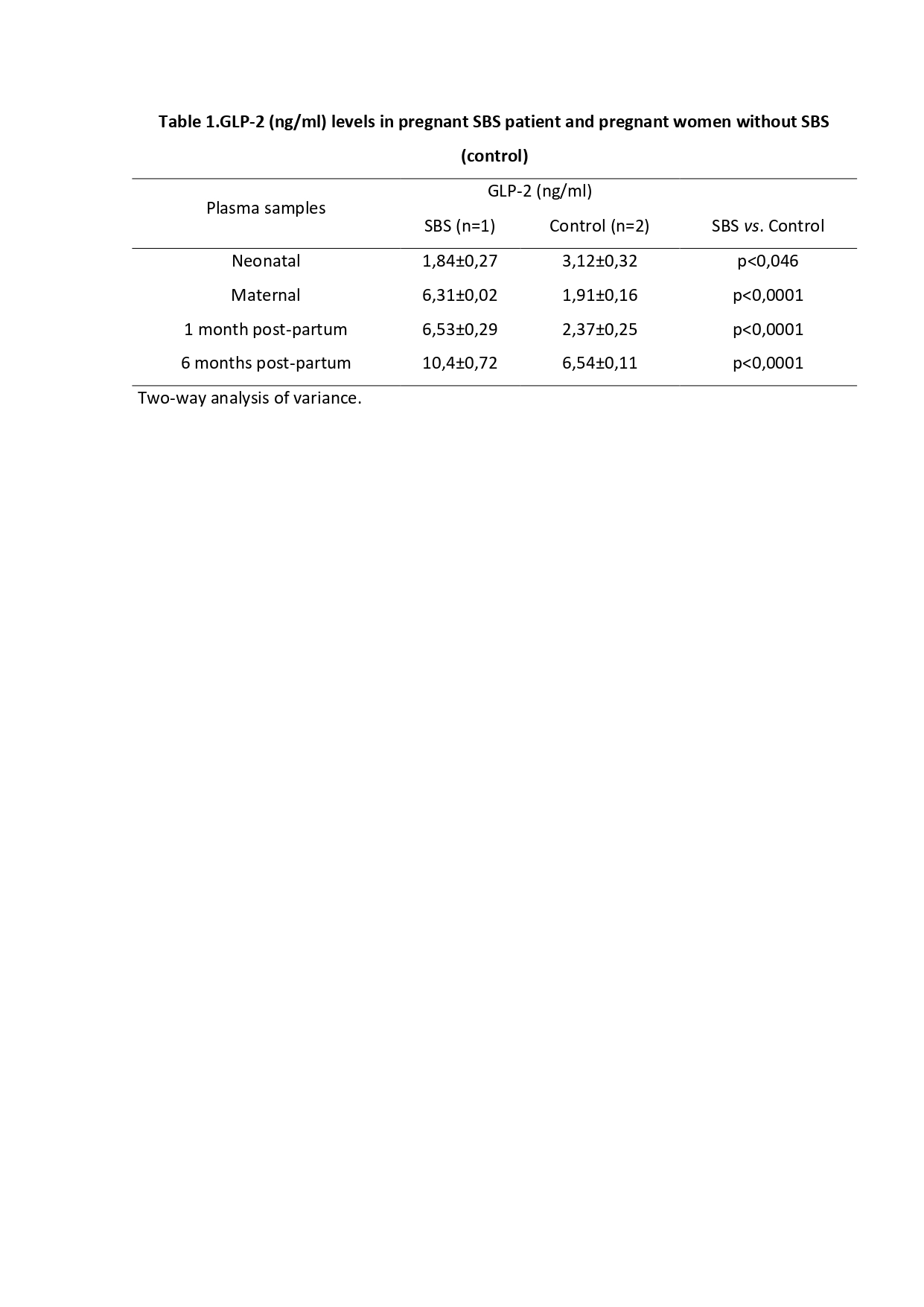
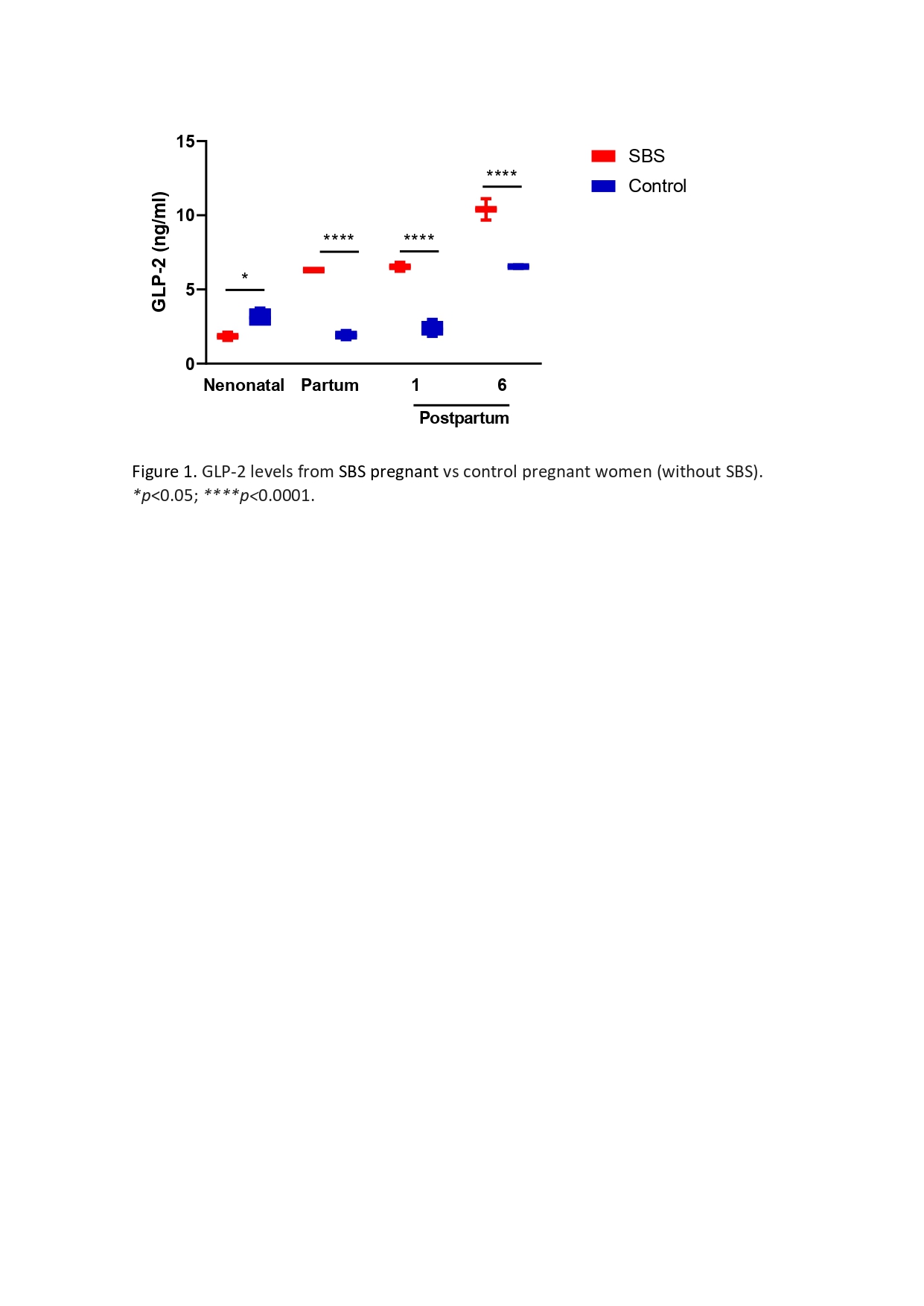
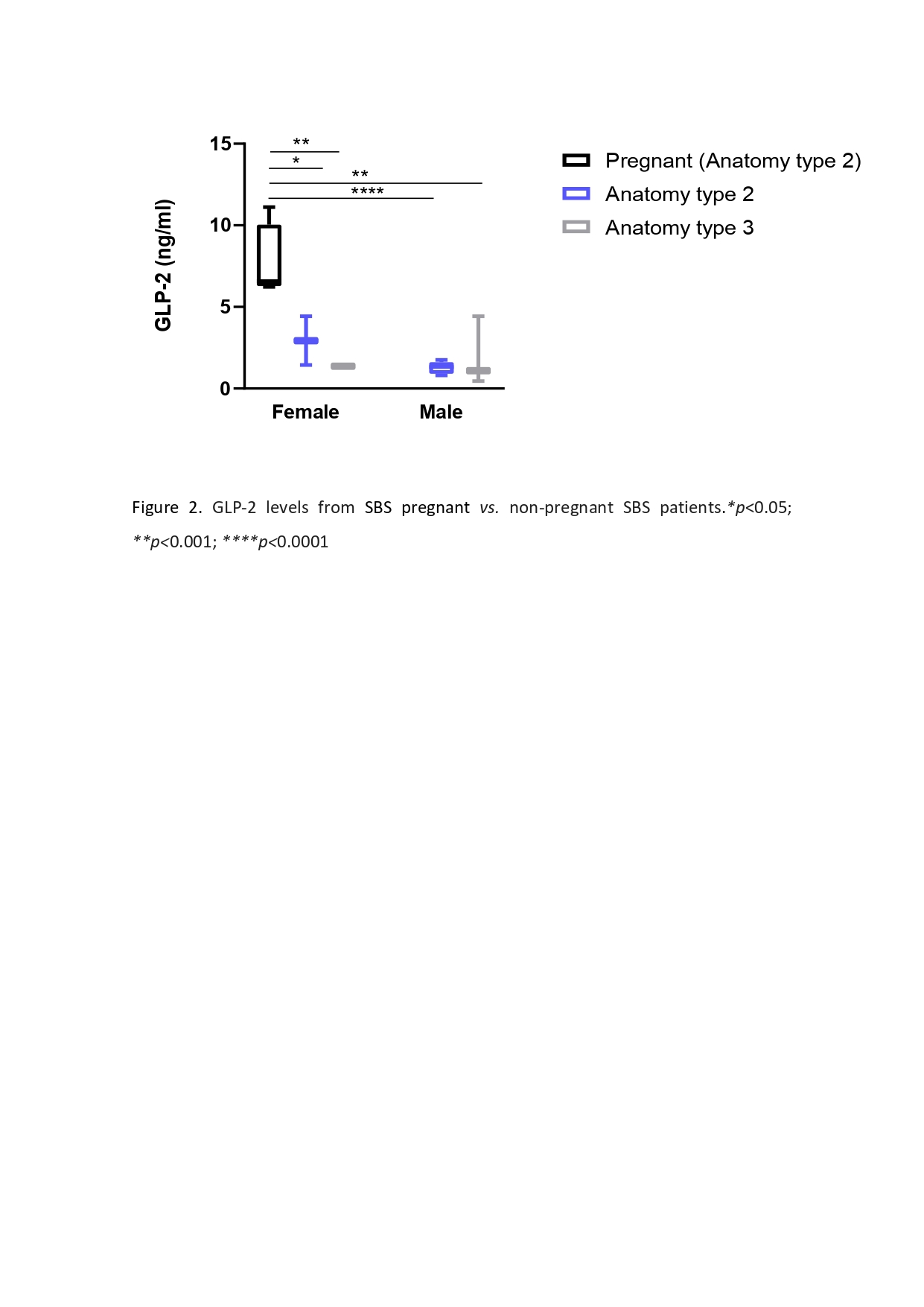
Case report: We report the case of a 33-year-old female patient with SBS/CIF (anatomy type 2), weaned off PN using sGLP-2. After 3.7 years of treatment, she became pregnant. The first decision was to interrupt the use of sGLP-2 as pregnancy is a contraindication for its use. She was able to successfully carry out the pregnancy to term without any additional PN support. She had adequate weight gain (59,0 to 66,15 kgs); the newborn weight was 2,450 kgs, and she was able to breastfeed her without complications. Our initial hypothesis was that endogenous fetal GLP-2 (eGLP2) levels could have been a sufficient source to maintain an adequate maternal intestinal absorption, if able to cross the placental barrier. Thus, during the pregnancy, we decided to determine eGLP-2 levels in paired neonatal (cord blood) and maternal plasma samples from pregnant with (n=1) or without SBS (controls, n=2) during the partum and the immediate breastfeeding period (1 and 6 months postpartum); we also aimed to measure and compare eGLP-2 plasma levels between pregnant (n=1) and a non-pregnant SBS patients (Anatomy type 2 (n=7); Anatomy type 3 (n= 5)).
Materials and Methods: Blood samples were collected in ice chilled 10 ml tubes containing ethylenediaminetetraacetic acid (EDTA) and a specific dipeptidyl peptidase IV inhibitor. Plasma was immediately separated and stored at −80°C until analyzed.
Results: Our results indicated that eGLP-2 levels were significantly lower in neonatal than maternal plasma from our pregnant SBS patient compared to controls (Table 1). During postpartum, eGLP-2 levels increased up to the six-month in both groups (Figure 1). Interestingly, our pregnant SBS patient showed significantly higher GLP-2 levels respect than controls (Figure 1) and non-pregnant SBS patients (Figure 2).
Conclusions: We observed that the endogenous neonatal GLP-2 does not represent an extra source of this entero-hormone to improve the adequate intestinal absorption during pregnancy in SBS patients. However, this study suggests that long periods of sGLP-2 treatment in SBS patients could reach an effective intestinal rehabilitation sufficient not only to improve intestinal absorption (to carry out the full pregnancy and to sustain breast feeding), but also to probably increase the eGLP-2 production. This study should be reproduced in experimental models and larger series to validate those results.
TAKEDA.
