Targeted delivery of galunisertib attenuates fibrogenesis in an integrated ex vivo renal transplant and fibrosis model
Leonie van Leeuwen1,2, Henri G.D. Leuvenink1, Benedikt M. Kessler2, Peter Olinga3, Mitchel J.R. Ruigrok3.
1Department of Surgery, University Medical Center Groningen, Groningen, Netherlands; 2Nuffield Department of Medicine, Centre for Medicines Discovery, Target Discovery Institute, University of Oxford, Oxford, United Kingdom; 3Department of Pharmaceutical Technology and Biopharmacy, Groningen Research Institute of Pharmacy, University of Groningen, Groningen, Netherlands
Background: Normothermic machine perfusion (NMP) is an emerging preservation technique for kidney allografts to reduce post-transplant complications, including interstitial fibrosis and tubular atrophy. This technique could be improved by adding antifibrotic molecules to perfusion solutions. We introduce a novel therapeutic approach, tested in a newly developed fibrosis model, to suppress fibrogenesis entitled Machine perfusion and Organ slices as a Platform for Ex vivo Drug delivery (MOPED). Our approach involves ex vivo perfusion with a blood based perfusate spiked with transforming growth factor beta (TGF-β) —one of the most important cytokines involved in fibrogenesis—and added galunisertib—a potent inhibitor of the TGF-β signalling pathway.
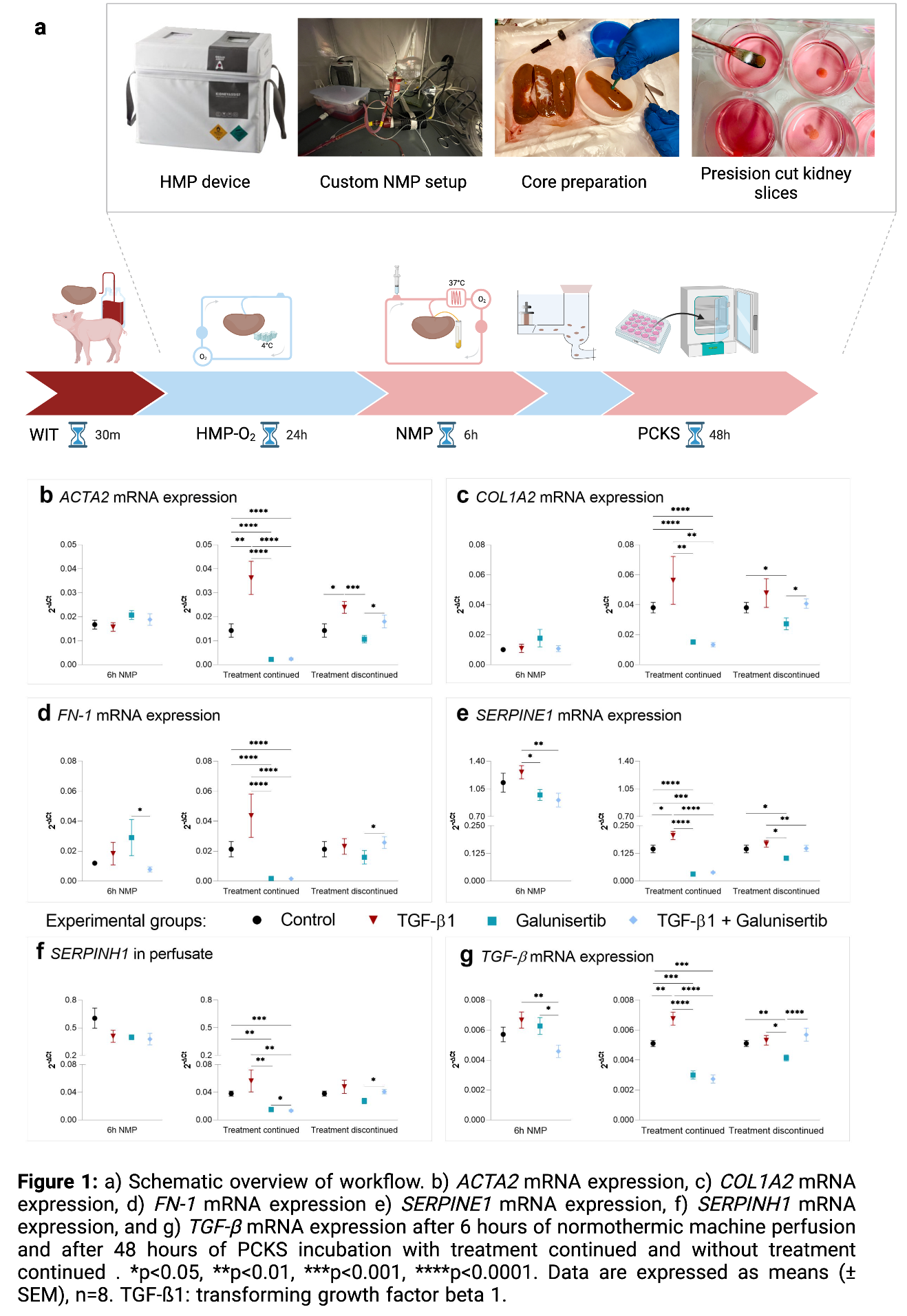
Methods: Porcine kidneys were subjected to 30min of warm ischemia, 24h of oxygenated hypothermic machine perfusion (HMP), and 6h of NMP with treatment (control, TFG-β, galunisertib, or TGF-β+galunisertib; n=8). To determine whether effects persisted upon ceasing treatment, precision-cut kidney slices (PCKS) were prepared from respective kidneys and incubated for 48h with treatment continued and discontinued (Figure 1a).
Results: Galunisertib supplementation improved the general viability, characterized by an increased oxygen consumption, elevated ATP levels and attenuated tubular dilation and necrosis. No significant differences in renal function, oxidative stress levels, or injury markers were observed. Galunisertib altered inflammation markers by causing a significant increase in gene expression of TNF-α, and a significant decrease of IL-6 after 6h NMP. This was supported by IL-6 protein expression. Continued TGF-β supplementation promoted fibrogenesis as shown by significantly increased mRNA expression of ACTA2, COL1A2, FN-1, SERPINE1, SERPINH1, and TGF-β after 48h of incubation. Continued treatment with galunisertib, however, clearly attenuated the expression of all tested fibrosis-related genes after 48h incubation (Figure 1b-g).
Conclusions: Our findings suggest that galunisertib positively affected mitochondrial activity, tissue integrity and expression of fibrogenesis-related genes, and therefore appears to be a promising drug for further research. These findings illustrate the value of targeted drug delivery using isolated organ perfusion for reducing post-transplant complications.
This work was funded by the Graduate School of Medical Sciences, and the Groningen Research Institute of Pharmacy, University of Groningen.
