Ibrahim Adam, Canada has been granted the TTS-CST International Transplantation Science Mentee-Mentor Awards
The role of role of sex and T cells in natural vs induced ABO antibody production in mice
Ibrahim Adam1,3,5,6, Bruce Motyka1,5, Kesheng Tao1,5, Peter J. Cowan7, Lori J. West1,2,3,4,5,6.
1Pediatrics, University of Alberta, Edmonton, AB, Canada; 2Surgery, University of Alberta, Edmonton, AB, Canada; 3Medical Microbiology and Immunology, University of Alberta, Edmonton, AB, Canada; 4Pathology and Laboratory Medicine, University of Alberta, Edmonton, AB, Canada; 5Alberta Transplant Institute, University of Alberta, Edmonton, AB, Canada; 6Canadian Donation and Transplantation Research Program, University of Alberta, Edmonton, AB, Canada; 7Immunology Research Centre at St. Vincent’s Hospital, University of Melbourne, Melbourne, Australia
Introduction: Interaction of ‘natural’ ABO antibodies (nAbs) with their cognate AB(H)-antigens (Ags) poses a high risk of rapid rejection of ABO-incompatible (ABOi) organ transplants. We previously demonstrated that a clear understanding of factors influencing ABO nAbs is crucial for successful ABOi heart transplantation. Here we investigated anti-A nAbs vs. intentionally.
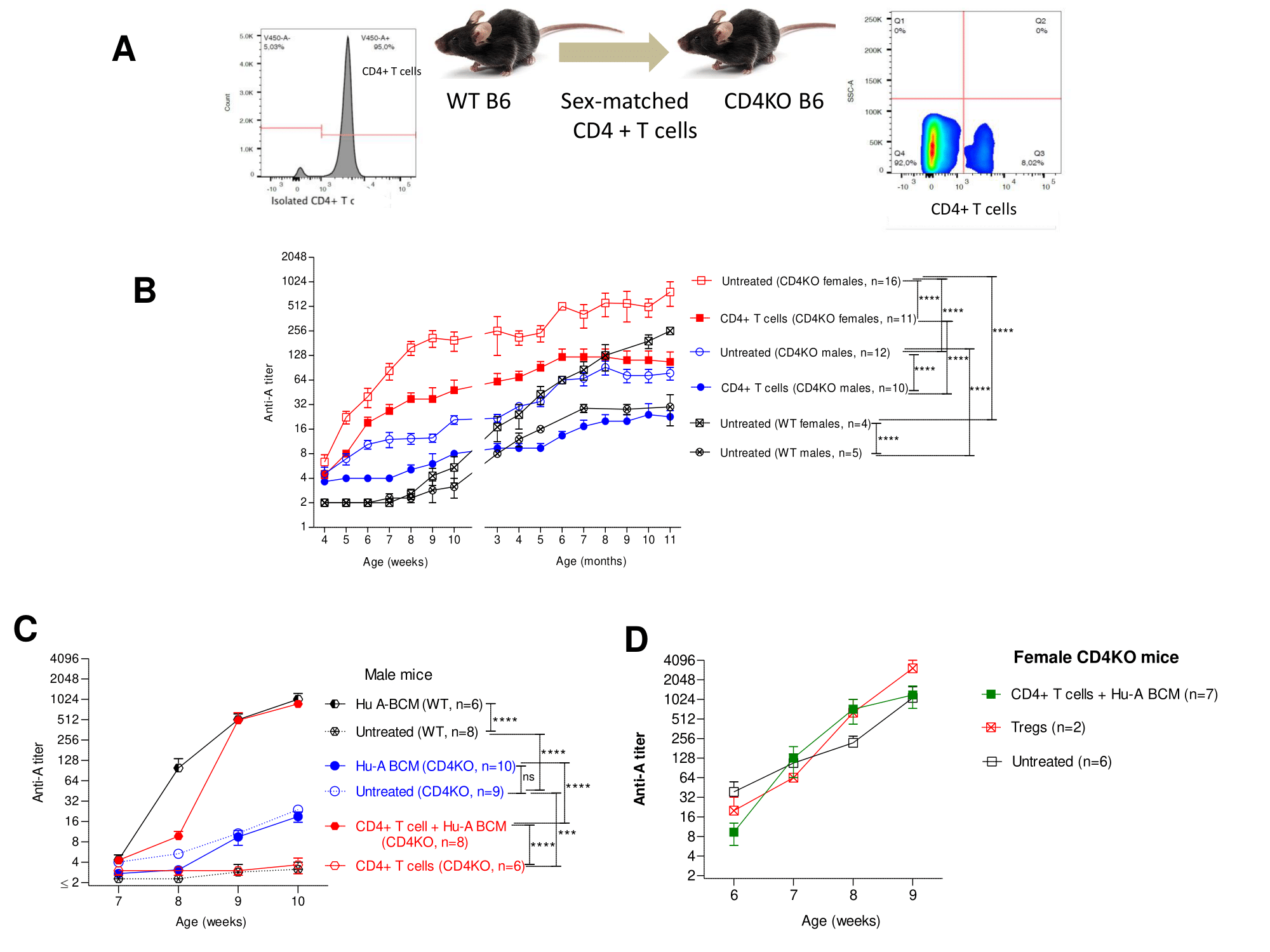
Methods: Adult wild-type (WT) and CD4 T cell knock-out (CD4KO) mice (C57BL/6 (B6) background) received weekly i.p. injection x3 of human ABO-A blood cell membranes (Hu-A BCM; 100ul of 10% v/v) or left untreated. Serum anti-A Ab was measured by hemagglutination assay using ABO-A erythrocytes from our A-transgenic mouse line. To test for T cell help and/or suppression, sex-matched CD4+ T cells (8-12×106/mouse) or CD4+CD25+ T cells (1.7-2.8×106/mouse) from spleens of WT mice were transferred to CD4KO mice. After adoptive transfer, CD4+ T cell reconstitution in peripheral blood was confirmed and mice were left untreated or challenged with Hu-A BCM and assessed for anti-A Ab.
Results: In contrast to WT mice, untreated CD4KO females produced dramatically more anti-A than males, rising substantially with puberty, and this was significantly suppressed in both sexes by adoptive transfer of sex-matched CD4+ T cells. Unlike WT mice, attempted sensitization of CD4KO mice with Hu-A BCM failed to induce additional anti-A beyond the already high levels in either sex; CD4+ T cell adoptive transfer rendered CD4KO mice responsive to A-sensitization. CD4+CD25+ T cell transfer into CD4KO mice neither suppressed anti-A nAbs nor rendered them responsive to A-sensitization (Figure).
Conclusions: When ABO ‘natural’ antibodies are discriminated from intentionally induced Abs, several important findings emerge: 1) Anti-A nAbs are produced without CD4+ T cell help in a sex- and age-dependent manner, suggestive of a role for sex hormones in regulating anti-A nAbs. 2) CD4+ T cells, but not CD4+CD25+ regulatory T cells, down-regulate anti-A nAb production. 3) In contrast to anti-A nAbs, production of anti-A iAbs was CD4+ T cell-dependent without a sex bias.