Long-term experience of liver transplant combined with other organs: a single center analysis
María Reyes Toso1, Florencia Fernandez2, Silvina Yantorno1, Hector Solar3, Carolina Rumbo1, Diego Ramisch2, Pablo Farinelli2, Pablo Barros Schelotto2, Pablo Rafaelle4, Daniel Absi5, Alejandro Bertolotti5, Valeria Descalzi1, Gabriel Gondolesi2.
1Hepatology and Liver Transplant Unit, Fundación Favaloro, Ciudad Autónoma de Buenos Aires, Argentina; 2Hepato-Pancreato-Biliary Surgical and Multiorgan Transplant Unit, Fundación Favaloro, Ciudad Autónoma de Buenos Aires, Argentina; 3Nutritional Support and Intestinal Rehabilitation and Transplant Unit, Fundación Favaloro, Ciudad Autónoma de Buenos Aires, Argentina; 4Kidney Transplant Unit, Fundación Favaloro, Ciudad Autónoma de Buenos Aires, Argentina; 5Intrathoracic Transplant Unit, Fundación Favaloro, Ciudad Autónoma de Buenos Aires, Argentina
Introduction: Until a few years ago, combined liver transplantation with other organs (SLT+O) was unusual and limited not only by the small number of patients with this indication, but also by the lack of trained transplant centers. The scarce number of manuscripts reporting indications, benefits and long-term outcomes of a SLT+O, motivates our study.
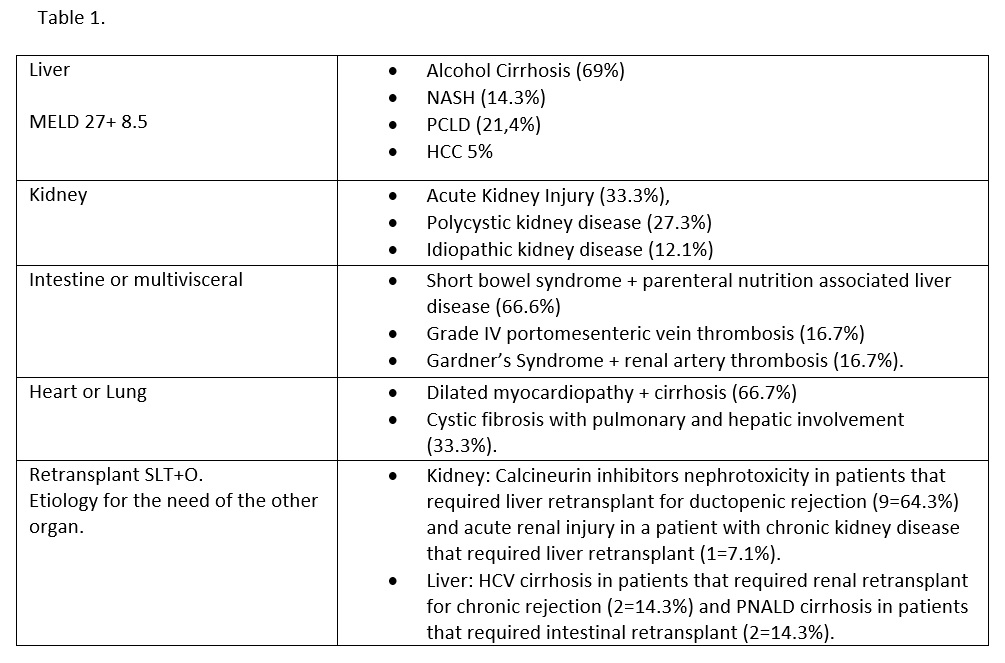
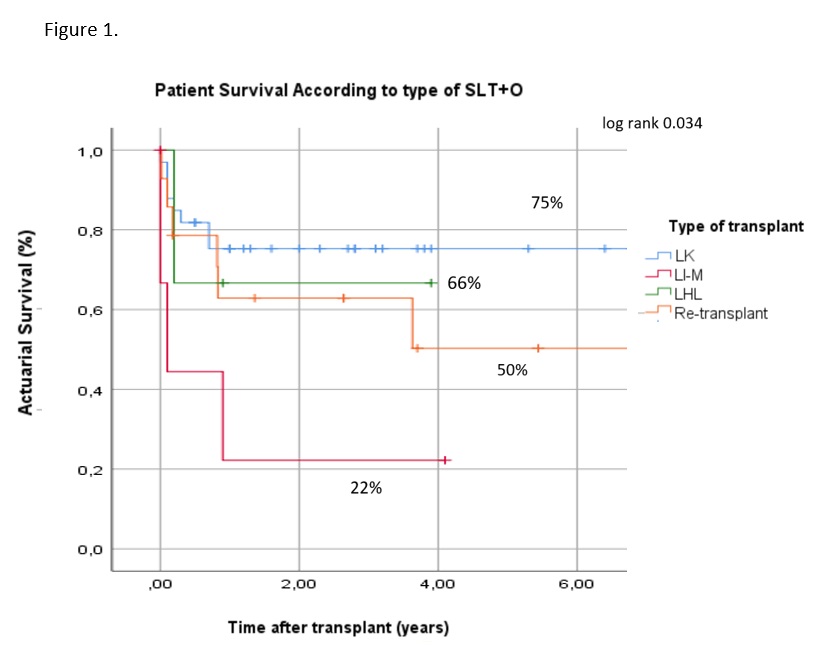
Patients and Methods: Between July 2009 and December 2021, 56 patients (pts) received a SLT+O in our center; 42 (75%) were primary and 14 (25%) were re-transplants. Pts were divided into 3 groups according to type of transplant (Tx): liver-kidney (LK), liver-intestine or multivisceral (LI-M), and liver-heart or liver-lung (LHL). A retrospective analysis was performed using clinical, immunological and Tx variables. Primary endpoints were pts and allografts survival. Statistical analysis: Chi square, T test, Kaplan Meier and log rank test. SPSS v20.0.
Results: 33/42 (78.5%) primary SLT+O pts received a LK, 6 (14.3%) a LI-M, and 3 (7.2%) a LHL Tx. All but 2 were adults, mean age 54 ± 15 years, 69% male; median follow up after Tx was 1.3 (0-12) years. Regarding the 14 re-transplants SLT+O, 12 were LK (85.7%) and 2 LI-M (14.3%), mean age 36 ± 18 years, 71% male; median follow up after Tx was 2 (0-12) years. Main indication for SLT+O (primary or re-transplants) are listed in table 1. Regarding primary SLT+O actuarial survival at 5 years was 75% for LK, 66% for LHL, and 22% for LI-M, while for re-transplant was 63% at 1 year and 50% at 5 years, log rank 0.034 (figure 1). No statistical difference was found on pt survival between primary vs re-transplant SLT+O. Regarding graft loss: for liver grafts, median survival was 1.2 (0-12) years; 2 patients required a 2nd liver transplant; 4 pts lost the K re-starting hemodialysis, and 1 required intestinal graft removal.
Conclusions: Combined transplantation is currently a feasible procedure as an indication of multi-organ failure. Over time, Tx programs face the challenge of offering these procedures increasingly. Current results and outcomes are comparable to single organ transplant under multidisciplinary multiorgan transplant institutes.