Use of donation after circulatory death donors for high model for end-stage liver disease recipients
Raphael Meier1,2, Miguel Nunez1, Shareef Syed1, Chris Freise1, John Roberts1, Nancy Ascher1, Ryutaro Hirose1, Garrett Roll1.
1Division of Transplant Surgery, Department of Surgery, University of California San Francisco, San Francisco, CA, United States; 2Department of Surgery, University of Maryland, Baltimore, Baltimore, MD, United States
Background: Donation after circulatory death (DCD) for liver transplantation (LT) remain an underutilized option in the United States, especially for the sickest end-stage liver disease patients. We hypothesized that recipients with a Model for End-Stage Liver Disease (MELD) ≥35 may have acceptable outcomes after DCD-LT.
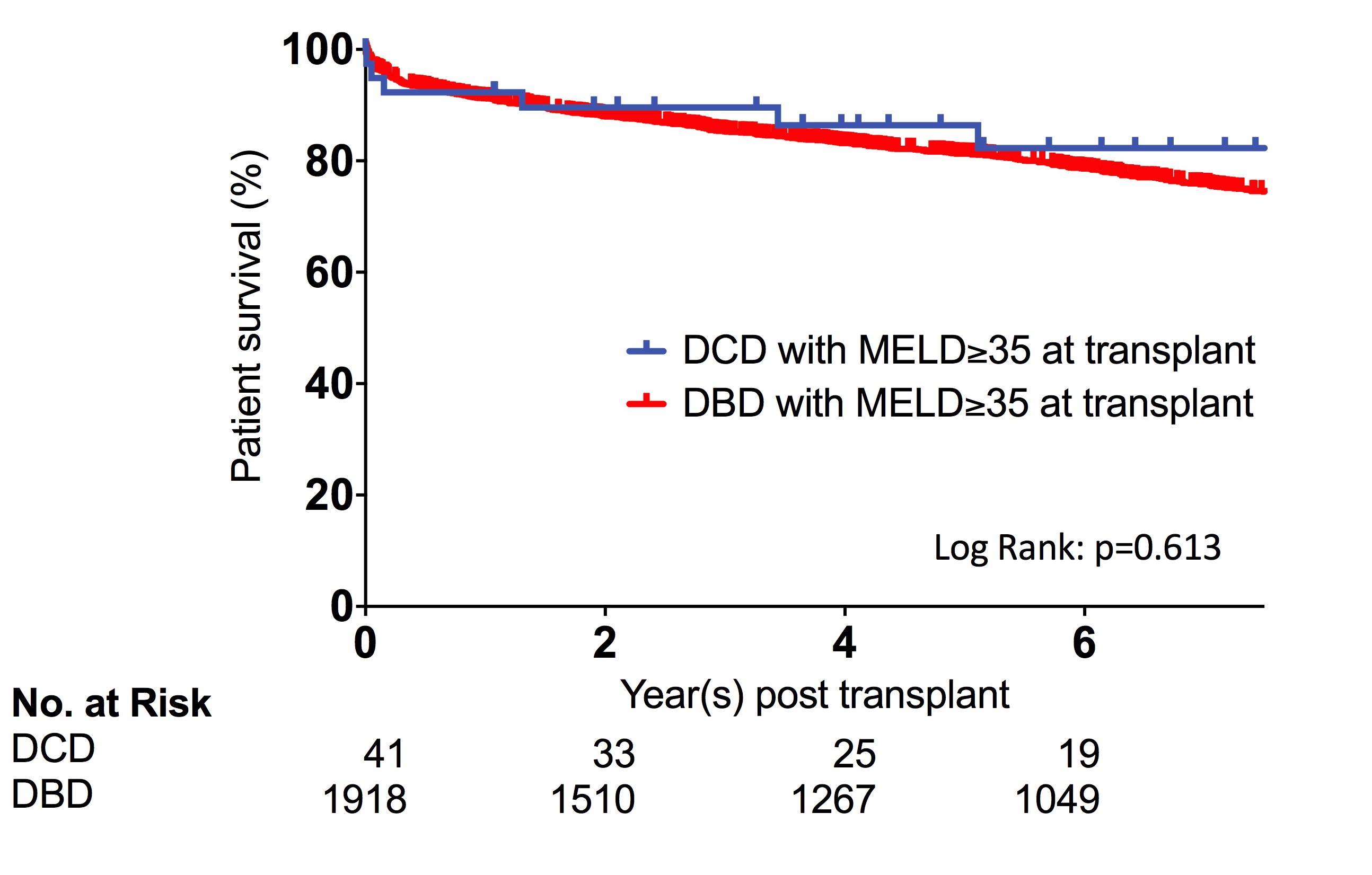
Methods: We collected and analyzed data on adult DCD recipients from the University of California, San Francisco (UCSF) cohort who had a lab-MELD of ≥35 at listing (n=41). No machine perfusion was used. We compared survival (Kaplan-Meier and Log Rank test) with our historical donation after brain death (DBD) recipients who had a lab-MELD of ≥35 at transplant (n=1,918).
Results: DCD recipient age (±SD) was 55.4 (8.8) years old, 63.4% were male, leading reasons for transplant were hepatitis C (34%) and alcoholic cirrhosis (27%). BMI (±SD) was 28.9 (6.6). All recipients were hospitalized prior to transplant, 46% were in the intensive care unit, and 51% were on renal replacement therapy at the time of transplant. 17% underwent a simultaneous liver-kidney transplant. Donor age was 31.1 (10) years, 63.4% were male, and the average BMI was 25.6 (6.8) kg/m2. Donor warm ischemia time was 21.0 (5.2) min, liver extraction time was 45.3 (19.3) min, and cold ischemia time was 7.8 (2.3) hours. The median length of stay post-transplant was 10 days. One patient out of four (26.8%) was on dialysis at discharge. DCD recipient's one-year survival was 92.3%, compared to 91.3% in DBD recipients, p=0.613 (Figure). 12.2% of the DCD recipients developed ischemic cholangiopathy.
Conclusion: DCD transplant in MELD of ≥35 recipients is feasible and can achieve similar one-year survival rates compared to DBD recipients with MELD≥35. Ischemic cholangiopathy remains present at an expected rate.