Is kidney time-zero biopsy useful to predict graft function at 1-year?
Daniela Wojtowicz1, Valeria Gabriela Alberton2, María Eugenia Zoppi1, Juan Santiago Rubio1, Silvia Di Pietrantonio1.
1Servicio de Nefrología y Trasplante Renal, Hospital de Alta Complejidad El Cruce Nestor Kirchner, Florencio Varela, Argentina; 2Servicio de Anatomía Patológica, Hospital de Alta Complejidad El Cruce Nestor Kirchner, Florencio Varela, Argentina
Introduction: Clinical and histological characteristics of donors are known to influence graft outcome after kidney transplantation. One of the most common reasons for donor kidney discard is unfavorable histology on procurement biopsies. Many centers perform time-zero biopsies (Bx0), although there is no consensus about the histological findings significance or its association with post-transplant biopsies results. We aim to determine if findings in Bx0 could predict the allograft function at 1-year after transplantation.
Methods: Adult kidney-transplant patients from October 2014 to December 2020 with Bx0, post-transplant biopsy performed and at least 1-year follow-up were included. Recipient’s gender and age, clinical donor characteristics, histological findings in Bx0 and post-transplant biopsies and 1-year creatinine levels were analyzed using SPSS® V.25.
Results: During the analyzed period 138 kidney transplants were performed. Bx0 was performed in 68 (49%) patients, and of those, 60 patients (88%) had at least one post-transplant biopsy. Mean age was 46 ± 14-year-old and 37 (54%) were male. Fifty-three patients (78%) received a kidney from deceased donor and 15 (22%) from living donor. Donor mean age was 43 ± 13-year-old. Fourteen (20%) had hypertension and the mean body mass index (BMI) was 27.3 ± 5.1 kg/m2. Donor’s mean serum creatinine before procurement surgery was 1.14 ± 0.53 mg/dL and the mean cold ischemia time (CIT) was 17:21 ± 9:40hs. Bx0 histological findings were: acute tubular necrosis (ATN) in 62 biopsies (19%), glomerulosclerosis (GS) in 40 (59%) and interstitial fibrosis and tubular atrophy (IFTA) in 41 (60%), with a mean of 6 ± 9% and 5 ± 7% respectively; 15 (22%) had arteriolar hyaline thickening. A risk factor for allograft GS was donor’s age >43-year-old (OR 4.4 95%IC 1.7 – 11.7 p= 0.000). In addition, we found that donor’s age >43-year-old and history of hypertension were risk factors for IFTA (OR 3.7 95%CI 1.6 – 8.8 p= 0.000 and OR 2.57 95%CI 1.4 – 4.4 p= 0.004 respectively). The mean of 1-year serum creatinine was 1.8 ± 1.6 mg/dL. Clinical and pathological parameter effects on 1-year serum creatinine are shown in table 1. The risk factors for worse outcomes in terms of 1-year serum creatinine are shown in table 2. We also found that GS and IFTA persist in post-transplant biopsies in 85% and 100% of patients respectively.
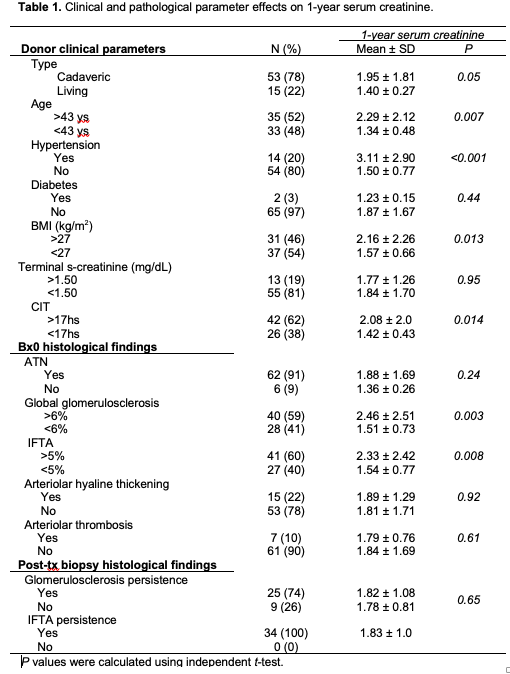
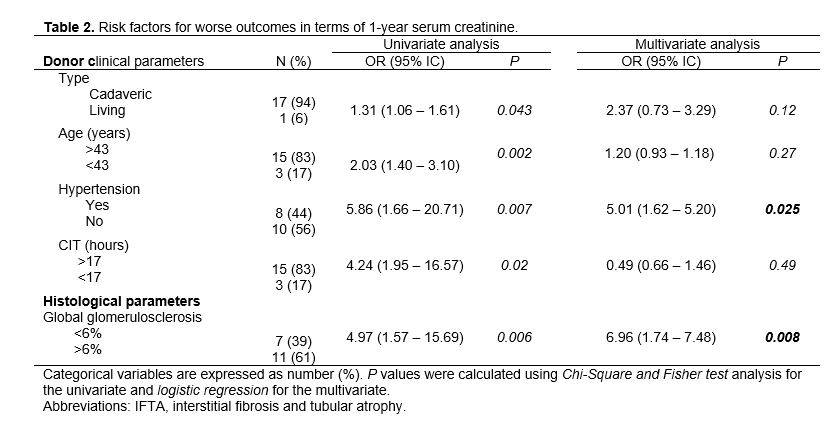
Conclusion: We have found that not only donor age and hypertension are risk factors for pathological findings in Bx0 but also those findings impact negatively on 1-year serum creatinine.
