Effects of exposure to sensitizing factors and degree of pre-transplant sensitization in the prognosis of kidney graft
Mayra Huanca Laura1, Luis Eduardo Dr Morales Buenrostro Dr1, Lluvia Aurora Marino Vazquez 1.
1Departamento de Nefrología de trasplante, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, México, , Mexico
Introduction: Renal transplant success is affected by several long-term events; the main cause of graft loss is antibody-mediated rejection. These rejection events will occur more frequently the greater the pre-transplant immunological risk, which depends largely on the presence of anti-HLA antibodies (HLA-Ab) directed at the donor due to previous exposure to sensitizing factors. The impact of natural HLA-Ab (pretransplant HLA-Ab without exposure to sensitizing factors) has not been clarified. A better understanding of the risk groups, would help us to give us guidelines for the management of long-term immunosuppression. The objective of this study was to compare the immunological outcomes and graft survival according to exposure to sensitizing factors and the presence of pre-transplant HLA-Ab in kidney transplant recipients.
Methods: Retrospective study that included transplanted patients between January 2014 and December 2015. Four groups were compared, based on exposure to sensitizing factors and the presence of pre-transplant HLA-Ab. The relevant outcomes to be analyzed between the 4 groups were: generation of post-transplant DSAs, acute rejections, graft loss and deaths.
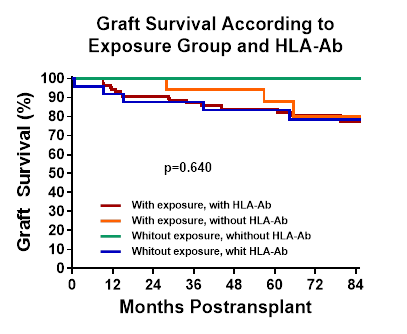
Results: 135 patients were evaluated, 51% female, with a mean age of 36±13 years. In patients with pre-transplant HLA-Ab, 50% had their persistence, and in patients without pre-transplant antibodies, 33% generated de novo HLA-Ab with a wider difference after the third year. The last control shows us that more than 50% of patients with HLA-Ab before transplantation and with exposure to sensitizing factors. The AMR events were more frequent among the groups with pre-transplant HLA-Ab of 37% and 36% with and without exposure to sensitizing factors, respectively and followed by the group with exposure to sensitizing factors and without HLA-Ab of 24%. As expected, the importance of post-transplant DSA in the incidence of AMR is highlighted.The groups with HLA-Ab before transplant, regardless of exposure to sensitizing factors, show a trend to lower graft survival, although it does not reach statistical significance (p=0.067).
Conclusion: This study shows a negative impact of the presence of HLA-Ab before transplantation including natural HLA-Ab. Therefore, it is essential to carry out compatibility studies and measurement of HLA-Ab before transplantation for adequate stratification of immunological risk, in addition to post-transplant monitoring of antibodies as a useful and effective surveillance tool.
