Accessibility to the kidney transplantation beyond immunology
Eulalia Sola Porta2, Wisam Bitar1, Jaakko Helve1, Patrik Finne1, Fernanda Ortiz1.
1Abdominal center, Nephrology, Helsinki University Hospital, Helsinki, Finland; 2Nephrology, Hospital del Mar, Barcelona, Spain
Background: Kidney transplantation (KT) has proven to be the preferable kidney replacement therapy (KRT) as it provides a better survival and quality of life. Well-known patient-related factors influencing patients’ access to KT are blood type, age, comorbidities, and pre-sensitization to HLA antigens. Research on home dialysis modalities´ effect on this matter is scarce.
Methods: We included all adult patients who started kidney replacement therapy (KRT) between 2004 and 2017 in the Helsinki University Hospital treated with home dialysis modalities (N=536), including home hemodialysis (HHD) and peritoneal dialysis; both CAPD and APD. A control group of in-center HD (ICHD) patients was randomly selected (N=200). The patients were followed-up until kidney transplantation, death, or end of follow-up in December 2020. We retrieved from registries variables with a potential effect on access to transplantation, of special interest we considered dialysis modality at 90 days after initiating KRT.
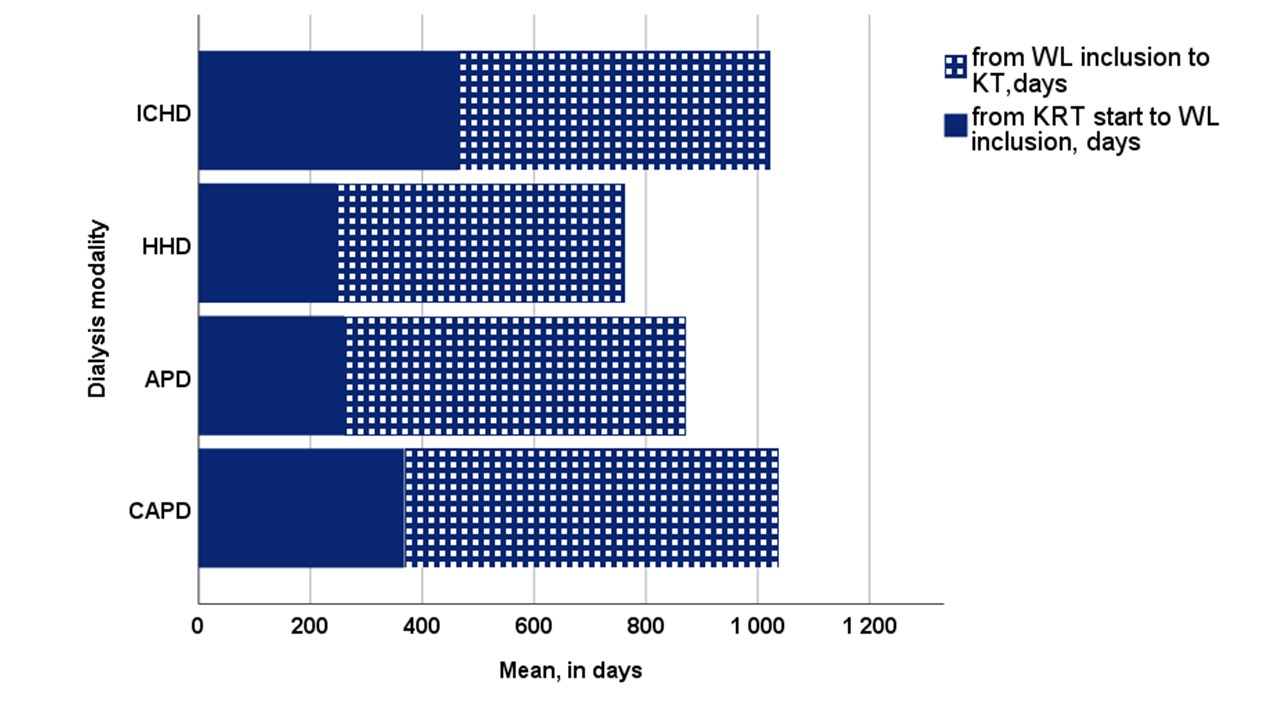
Results: In all, 481 out of 736 patients were waitlisted for kidney transplantation, of whom 423 were transplanted (88%), 23 patients (5%) died on the waitlist (WL), 24 were permanently removed from the WL (5%) and 11 were still on the WL at the end of FU. The probability of waitlisting was 2.1 as high in CAPD patients (p=0.004), and 7.9 times as high in both APD and HHD patients (p<0.001) compared to ICHD. Cardiovascular morbidity did not affect waitlisting. Of those who were waitlisted, both ICHD (N=74) and CAPD (N=80) patients were older than APD (N=199) and HHD (N=128) patients (mean age 54; 56; 48 and 49 YO respectively). Mean (95% CI) time elapsed from KRT initiation to WL inclusion was 307 days (251-362), time from WL to KT was 458 days (542-636) and time off the WL due to an intercurrence was 96 days (80-112). There were no differences between dialysis modalities in terms of time from WL to KT (p=0.176), but time to WL was significantly longer in ICHD patients (p=0.014) (Figure 1) The time off the WL equally delayed KT irrespective of the dialysis mode. (p=0.141)
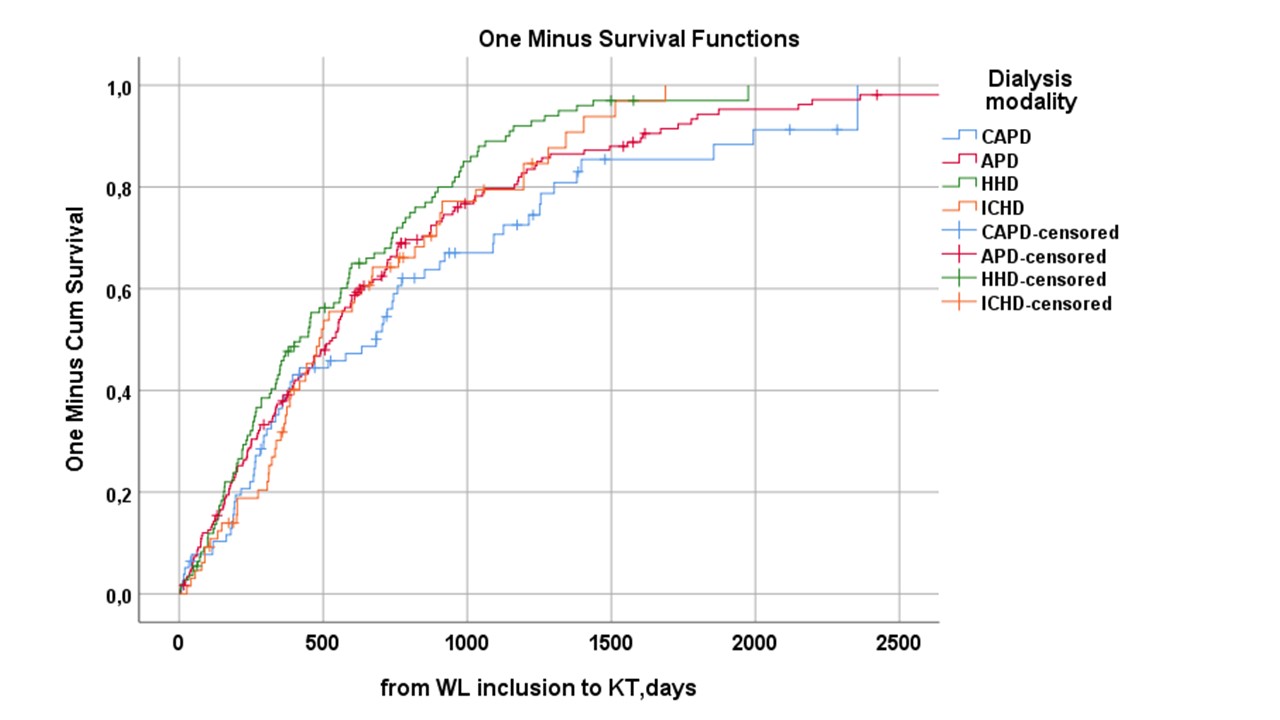
Dialysis modalities had an impact on the time elapsed from WL to KT (log rank p=0.028). (Figure 2) By Cox regression analysis the variables that were significantly related with the outcome were panel reactive antibodies type 1 (p=0.033), and time off the WL (p<0.001), while cardiovascular comorbidity (p=0.246), dialysis modality (p=0.208), malignancy (p=0.675), panel reactive antibodies type 2 (p=0.679) and age (p=0.054) did not reach the level of significance. Altogether 732 episodes resulted in the patients being temporarily removed from the WL, and the most common reasons were PD-peritonitis (20%), other infections (26%), and surgery/dental treatment (10%). On the other hand, both vascular access complications (1%) and cardiovascular intercurrences (4.9%) were uncommon.
Conclusions: Dialysis modality significantly influences patients’ access to transplantation. APD and HHD modalities provided a benefit in terms of accessing the WL. In patients wait listed, intercurrent complications during dialysis, mainly infections, significantly prolonged the waiting time for KT in all patients beyond immunological reasons.
