Outcome analysis of patients with genetic mutations of complement regulatory proteins in relation to incidence of post renal transplant thrombotic microangiopathy
Ankur Mittal1, Abhijit Konnur1, Sishir Gang1, Mohan Rajapurkar1, Umapati Hegde1, Hardik Patel1, Shailesh Soni2, Sachidanand Panday2.
1Nephrology, Muljibhai Patel Urological hospital, Nadiad, India; 2Pathology, Muljibhai Patel Urological hospital, Nadiad, India
Introduction: Thrombotic Microangiopathy is an occlusive disorder of microvasculature characterized by thrombocytopenia, systemic or intrarenal platelet aggregation, thrombus formation and hemolytic anemia caused by fragmentation of erythrocytes due to the disturbed microvasculature. TMA developing after renal transplantation can be categorized into either De novo TMA, developing for the first time without any evidence of the disease before the transplant or recurrent TMA where native kidneys have failed due to TMA and recur after kidney transplantation. The contribution of complement regulatory gene (CRG) mutation to post-transplant Thrombotic Microangiopathy (TMA) in Indian kidney transplant recipients (KTR) is unknown. This is a study to determine the association of CRG on post-transplant TMA and graft failure.
Methods: A Single Centre, Prospective Observational Cohort Study was undertaken in renal transplant recipients. All live and Deceased donor renal allograft recipients who underwent transplantation from 1st December 2019 onwards till 31st December 2020 were recruited and were followed up for 1 year beyond the last enrolment. Genetic testing was performed with MLPA and Clinical exome sequencing.
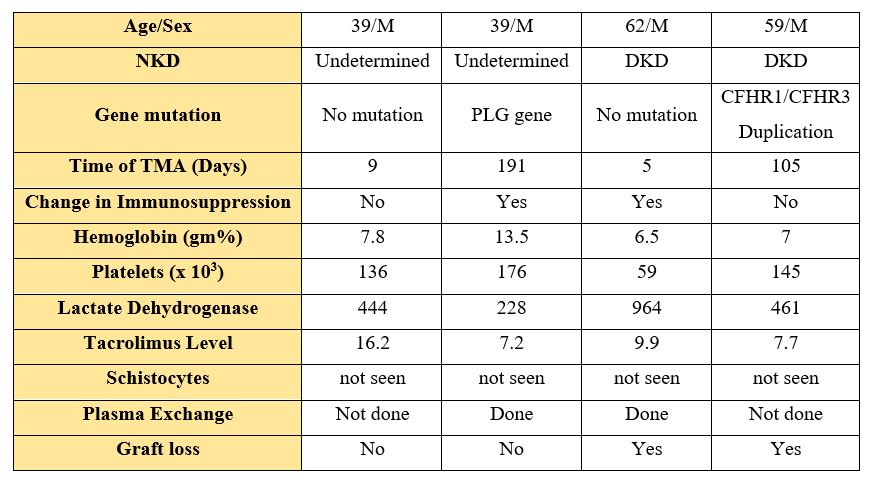
Results: 78 KTRs with a mean age of 37.09 ± 13.23 years were enrolled. The Native cause of kidney disease in 55 (70.5%) patients was undetermined and 23 (29.5%) had established cause of chronic kidney disease. 58 (74.4%) were males and 20 (25.6%) were females. CRG mutation was seen in 48/78 (61.5%) KTRs. The allele frequency of the CRG mutation was seen in 48/78 (61.53%) of which duplication of CFHR gene was predominantly seen in 40/78 (51.2%) patients. CRG mutation in this cohort was seen more in the younger age group patients. There was no gender predominance for patients with CRG mutation. None of the patients had a mutation for CFH, CFI, CFB, C3, THBD, DGKE genes. One patient had a mutation for the PLG gene. The incidence of post-transplant TMA was seen in 4/78 (5.12%) patients. Mutation related to aHUS was seen in 2 patients.
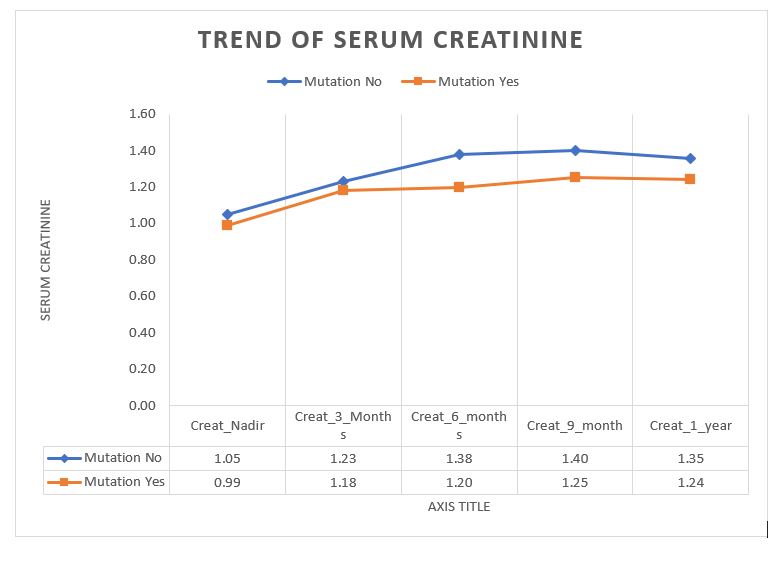
There was no significant difference in serum creatinine levels of patients with or without CRG mutation at the end of 1 year.
Conclusion: The prevalence of CRG mutation in our KTR cohort was high and is associated with post-transplant TMA in 50% of patients with de novo TMA. The graft outcome at the end of 1 year was similar in patients with mutation and those without mutation. This study suggests that the presence of CRG mutation should not preclude renal transplantation in patients with ESRD.
