Influence of CIT-induced DGF on transplant outcomes among DCD kidneys
Nikolas Zaphiros1,2, Jing Nie3, Liise K Kayler1,2,4.
1Department of Surgery, University at Buffalo, Buffalo, NY, United States; 2Transplant and Kidney Care Regional Center of Excellence, Erie County Medical Center, Buffalo, NY, United States; 3Department of Epidemiology and Environmental Health, University at Buffalo School of Public Health and Health Professions, Buffalo, NY, United States; 4Jacobs School of Medicine and Biomedical Sciences, University at Buffalo , Buffalo, NY, United States
Background: Donation after circulatory death (DCD) kidneys are exposed to ischemic events from withdrawal of support, which when coupled with increased cold ischemia time (CIT) predisposes to delayed graft function (DGF). DGF is considered a risk factor for graft failure after kidney transplantation. Clinicians may be reluctant to transplant DCD kidneys that also have prolonged CIT for fear of an additional deleterious effect.
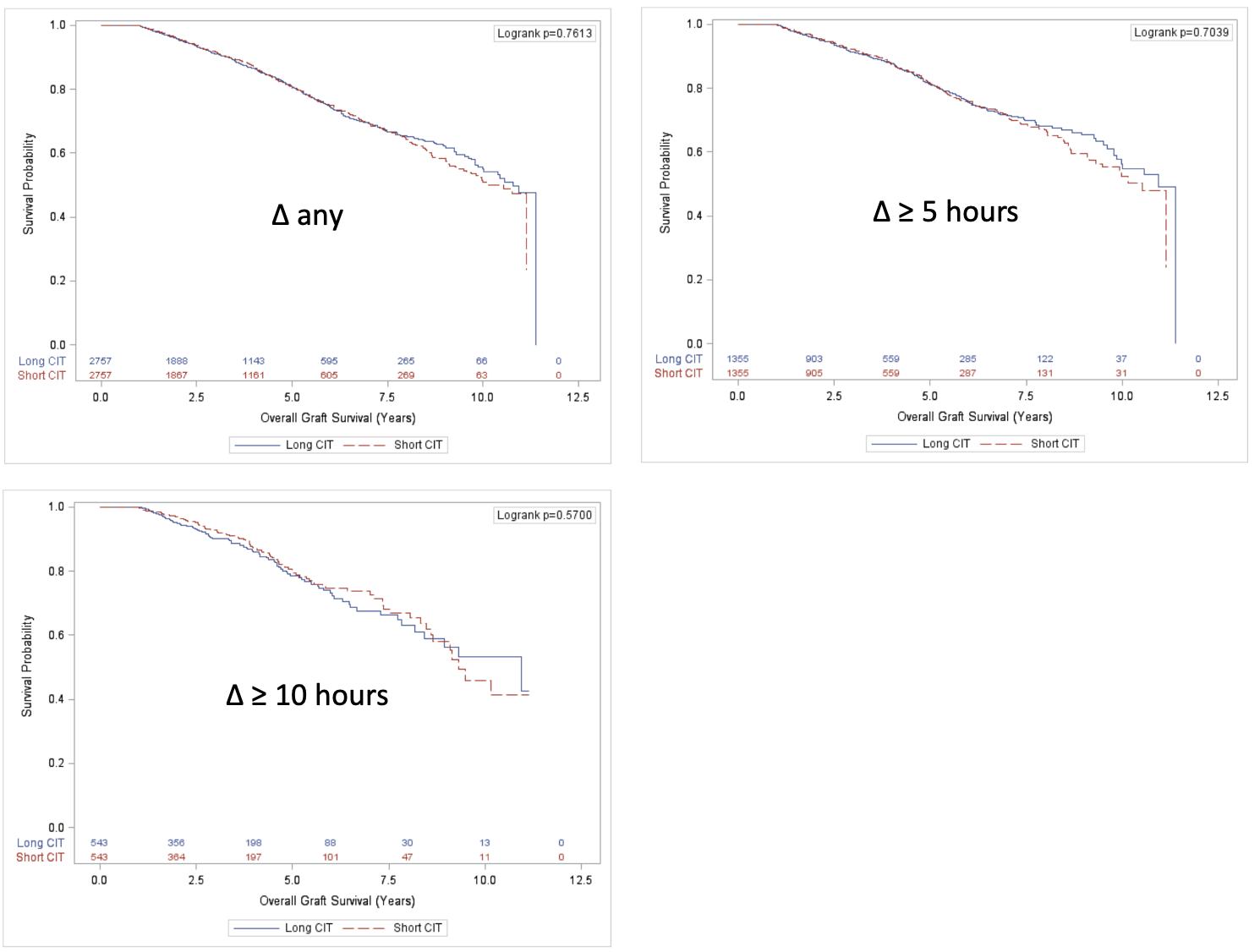
Methods: To analyze the risk of CIT-induced DGF on graft survival among DCD kidneys, we evaluated national data between 2008 and 2018 of adult first-time kidney-only recipients of paired kidneys from DCD donors, in which one donor resulted in DGF and the other did not. We evaluated outcomes where CIT difference between paired recipients was any, 5, or 10 hours.
Results: Out of 20,059 DCD recipients, 14,545 were excluded for mate kidney non-transplantation, both or neither kidney developed DGF, missing CIT, or mate kidney recipients with equal CIT. The remaining 5,514 paired kidney recipients (2,757 donors) were analyzed. All donor and recipient characteristics were similar except for more non-locally shared kidneys, greater HLA mismatch, and longer pre-transplant dialysis duration in the longer CIT group. On multivariate analysis of DCD kidney recipients, overall graft survival was comparable between recipients with higher CIT relative to paired donor recipients with lower CIT when a CIT difference was present (adjusted hazard ratio [aHR] 1.04, 95% CI 0.91 to 1.19, n=5,514), 5 hours (aHR 1.04, 95% CI 0.85 to 1.27, n=2,710), or 10 hours (aHR 0.88, 95% CI 0.65 to 1.21, n=1,086). Between each of the 3 delta-CIT levels of shorter and longer CIT, there were statistically significant differences in the proportion of delayed graft function at delta any, 5, or 10 hours.
Conclusions: These results suggest that in the setting of DCD kidney transplantation, DGF, specifically induced by prolonged CIT, has limited bearing on long-term outcomes. This may be important evidence that despite the occurrence of warm ischemic injury, kidneys with prolonged CIT offer acceptable outcomes to recipients and are a potential source to expand the donor pool.
Empire Clinical Research Investigator Program (ECRIP) of New York.
