Poor sleep quality, fatigue, social participation and health-related quality of life in kidney transplant recipients
Daan Kremer1, Tim J. Knobbe1, António W. Gomes-Neto1, Michele F. Eisenga1, Marco van Londen1, Rianne M. Douwes1, Coby Annema2, Ute Bültmann2, Ido P. Kema3, Gerjan J. Navis1, Stefan P. Berger1, Stephan JL Bakker1.
1Department of Internal Medicine, Division of Nephrology, University Medical Center Groningen, University of Groningen, Groningen, Netherlands; 2Department of Health Sciences, University Medical Center Groningen, University of Groningen, Groningen, Netherlands; 3Department of Laboratory Medicine Research, University Medical Center Groningen, University of Groningen, Groningen, Netherlands
TransplantLines Investigators.
Background: Fatigue and limited health-related quality of life (HRQoL) are common among kidney transplant recipients (KTR). We hypothesized that both may partly be attributable to poor sleep.
Methods: We used data of KTR (≥1 year after transplantation) and healthy controls (HC) from the TransplantLines Biobank and Cohort Study. Sleep quality was assessed using the validated Pittsburgh Sleep Quality Index. Determinants of poor sleep quality were identified using logistic regression. Associations of poor sleep quality with fatigue, societal participation, and HRQoL were assessed using linear regression. Among a subgroup of KTR, sleep quality was assessed before, at six and twelve months after transplantation, allowing to assess sleep quality trajectories over time.
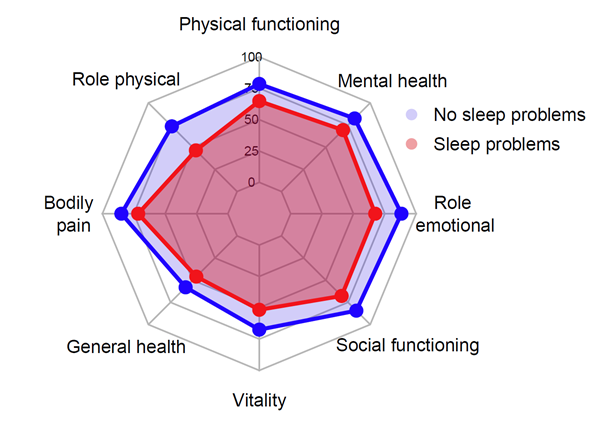
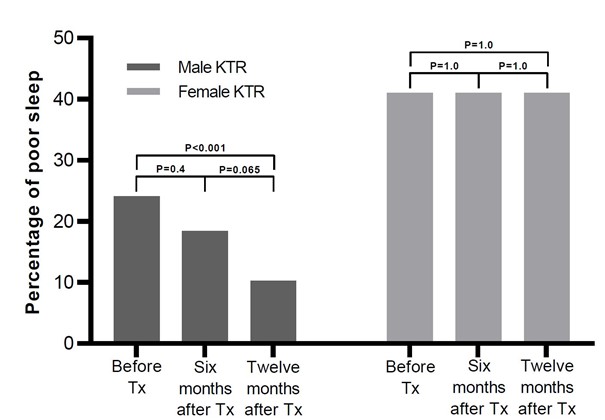
Results: We included 872 KTR (61.1% male, age 55.7±13.1y) with available data on sleep ≥1 year after transplantation, and 335 HC. In total, 16.7% of male KTR and 31.0% of female KTR reported poor sleep quality, which was significantly higher compared to HC (males: 8.8%, PChi-squared=0.017 and females: 15.5%, PChi-squared<0.001, (Figure 1). Next to female sex, more anxiety and calcineurin inhibitor usage were main determinants of poor sleep quality. Additional analyses suggested effect modification by age for the latter, and subgroup analyses confirmed that calcineurin inhibitors were associated with increased risk of poor sleep quality only in patients <57 years old (OR 6.14, 95%CI 1.87-20.15). Poor sleep quality was associated with more fatigue (st. β 0.34, P<0.001), lower ability to concentrate (st. β 0.27, P<0.001), poorer societal participation (restriction score: st. β -0.24, P<0.001), and lower HRQoL (physical component: st. β -0.32, P<0.001 and mental component: st. β -0.40, P<0.001, see Figure 2 for differences per subdomain of HRQoL) among KTR, which all remained independent of potential confounders. Longitudinal data in a subgroup of 124 participants showed that sleep quality improved after kidney transplantation in males (P<0.001), but not females (Figure 3).
Conclusion: Poor sleep quality is common among KTR. Additionally, these results highlight the clinical and personal importance of sleep quality and indicate that sleep may potentially be a key target to improve fatigue, societal participation, and HRQoL.

Astellas BV. Chiesi Pharmaceuticals BV.
