Urinary selenium excretion and long-term outcomes in stable kidney transplant recipients
Manuela Yepes Calderon1, Daan Kremer1, Adrian Post1, Ulrike Seidel2, Patricia Huebbe2, Tim J Knobbe1, Kai Lüersen2, Michele F Eisenga1, Gerjan J Navis1, Gerald Rimbach2, Stephan JL Bakker1.
1Nephrology, University Medical Center Groningen, Groningen, Netherlands; 2Institute of Human Nutrition and Food Science, University of Kiel, Kiel, Germany
TransplantLines.
Introduction: Although kidney transplantation is the best available treatment for end-stage kidney disease (ESKD), much room for improvement of long-term outcomes remains. One potential modifiable factor is the status of the essential trace element Selenium (Se), which must be obtained from diet, and is vital for promotion of antioxidant defence and inflammation regulation. Trace elements imbalance is common in patients with ESKD and on haemodialysis, and is not entirely corrected after kidney transplantation. We aimed to study whether Se status is associated with graft failure and mortality in kidney transplant recipients (KTR).
Methods: In this prospective cohort study, all adults KTR with a functioning graft for ≥1-year, without a history of addiction or malignancy, who visited the outpatient clinic of the University Medical Center of Groningen (The Netherlands) between November 2008–May 2011 were invited to participate. Twenty-four-hour urinary Se was chosen as the measurement for Se status since it is considered a trustful indicator of effective Se intake. All participants were asked to collect a 24-hour urine sample during the day before to their visit to the outpatient clinic and urinary Se was measured using inductively-coupled plasma mass spectrometry. The primary endpoints of the current study were all-cause mortality and graft failure. No participants were lost to follow-up. The association between urinary Se and outcomes was tested by means of Cox-proportional hazards regression analyses and restricted cubic splines for graphic purposes. For analyses IBM SPSS software and R Studio were used.
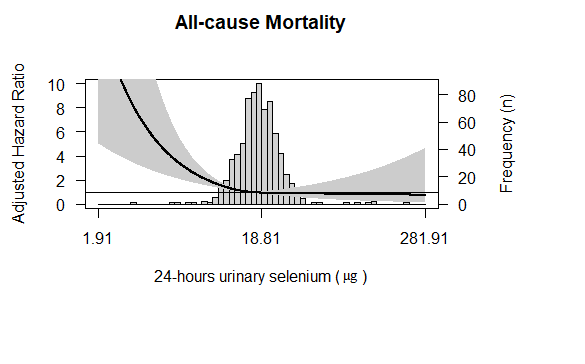
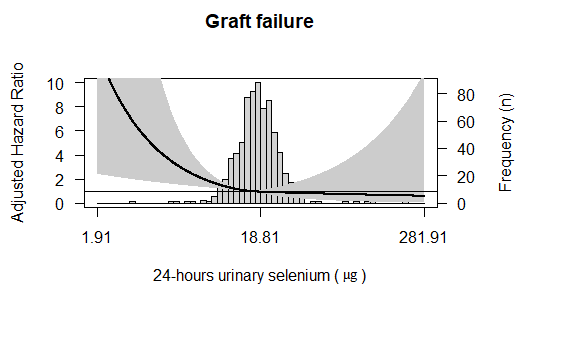
Results: A total of 693 stable KTR were included (mean age 53 ± 13 years, 57% male, 96% Caucasian) at a median of 5.39 [IQR, 1.97–12.04] years after transplantation, with a mean eGFR of 52 ± 20 mL/min/1.73m2. Median 24-hours urinary Se at baseline was 18.8 [IQR,15.1-23.4] µg. During a median follow-up of 5.4 [IQR 4.8–6.1] years, 150 (21%) died and 83 (12%) developed graft failure. Multivariable-adjusted analyses showed that 24-hour urinary Se excretion was associated with a lower risk of all-cause mortality (HR 0.72; 95% CI, 0.61-0.85 per 1-SD, P<0.001) and graft failure (HR 0.74; 95% CI, 0.59-0.92 per 1-SD, P=0.007) (Figure 1). The association of all-cause mortality with 24-hours urinary Se remained independent of adjustment for age, sex, and graft function (eGFR, proteinuria and 24-hours urinary volume), while this was not the case for graft failure (P=0.01 and P=0.36, respectively).
Conclusion: In a large cohort of stable KTR, 24-hours urinary Se was lower than reported for healthy individuals. Furthermore, Se excretion was inversely associated with the risk of long-term all-cause mortality and graft failure, and the association of all-cause mortality remained independent of baseline graft function. Further studies are warranted to elucidate whether Se-targeted interventions may improve long-term outcomes in KTR.
This study was based on the TransplantLines Food and Nutrition Biobank and Cohort Study (TxL-FN), which was funded by the Top Institute Food and Nutrition of the Netherlands (grant A-1003).
