Intestinal transplantation in a country without home parenteral nutrition; the largest report from the middle east
Hamed Nikoupour2, Mohammad Bagher Khosravi1, Pooya Vatankhah1, Mojtaba Shafiekhani3, Alireza Shamsaeefar2, Peyman Arasteh2, Mohammad Hossein Anbardar4, Mohammad Hossein Eghbal1, MohammadAli Sahmeddini1, Fatemeh Khalili1, Mohammad Firoozifar2, Samaneh Ghazanfar Tehran1, Saman Nikeghbalian2.
1Anesthesiology and Critical Care Research Center, Shiraz University of Medical Sciences, Shiraz, Iran (Islamic Republic of); 2Shiraz Transplant Center, Abu Ali Sina Hospital, Shiraz University of Medical Sciences, Shiraz, Iran (Islamic Republic of); 3Department of Clinical Pharmacy, Faculty of Pharmacy, Shiraz University of Medical Sciences, Shiraz, Iran (Islamic Republic of); 4Department of Pathology, Abu Ali Sina Hospital, Shiraz University of Medical Sciences, Shiraz, Iran (Islamic Republic of)
Background: Many regions of the world, especially middle and low income countries, lack facilities for home parenteral nutrition (HPN) and thus cannot follow existing guidelines for intestinal transplantation (ITx). Inhere we report our experiences with treatment protocols, intraoperative managements, and early postoperative outcomes among patients undergoing either isolated ITx or multivisceral transplantation (MVTx) in our center.
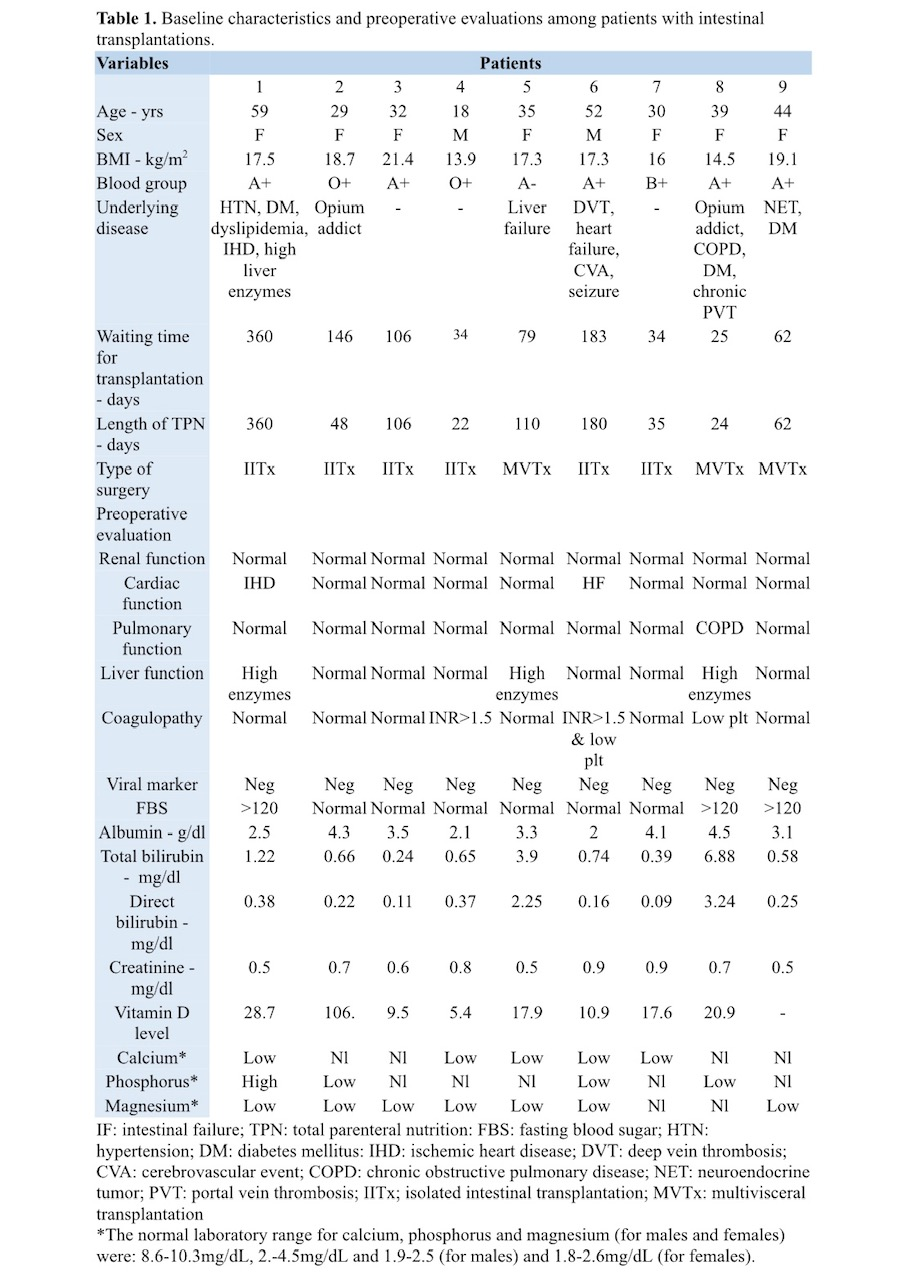
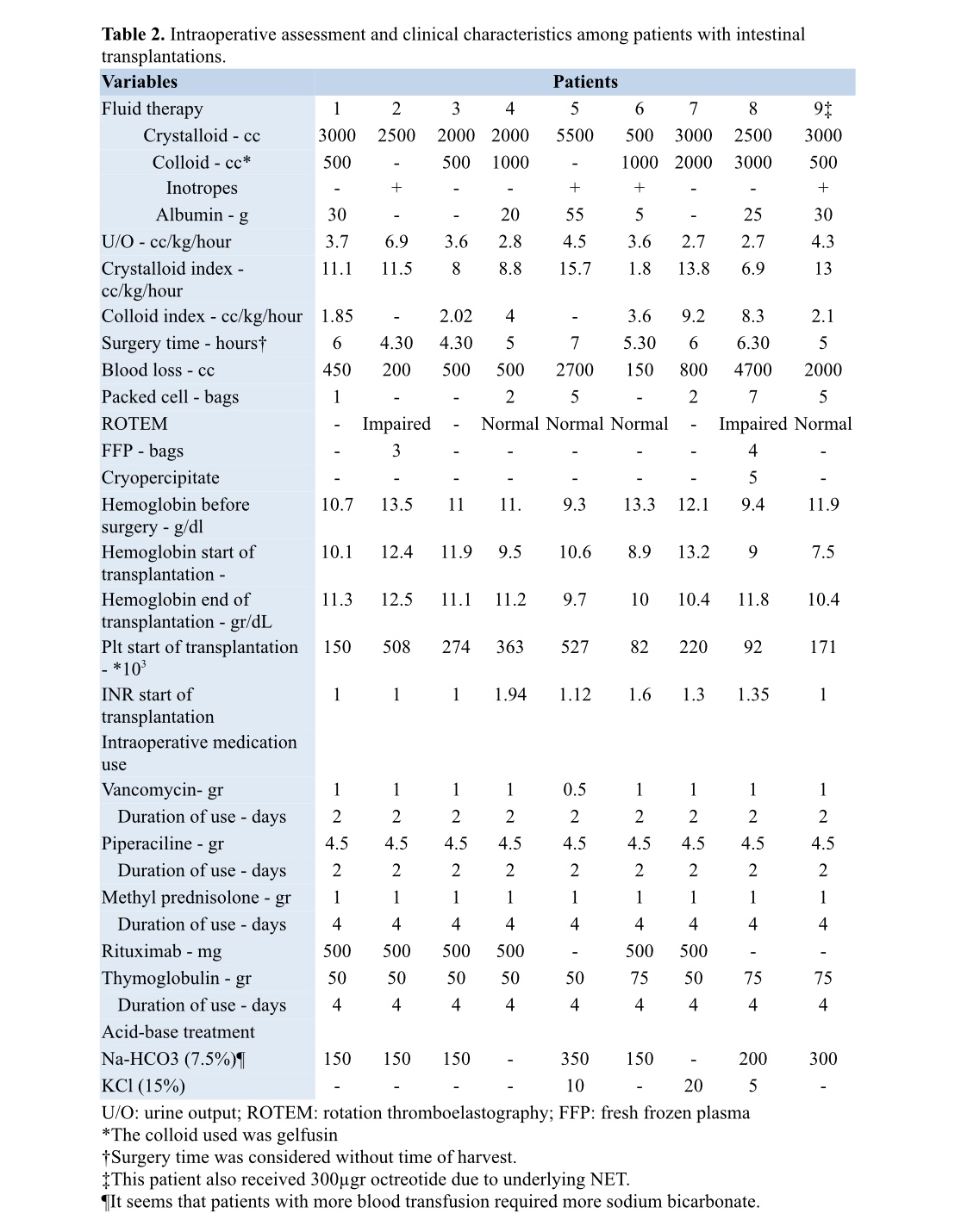
Methods: In the Shiraz Transplant Center, during a one year period from March 2019 up to March 2020, a total of nine ITxs have been performed, including six isolated ITxs and three multivisceral transplantations (MVTx). We reported on donor selection strategies, surgical treatment, anesthesiology care and protocols for total parenteral nutrition, immunosuppression regimen and pathology evaluation.
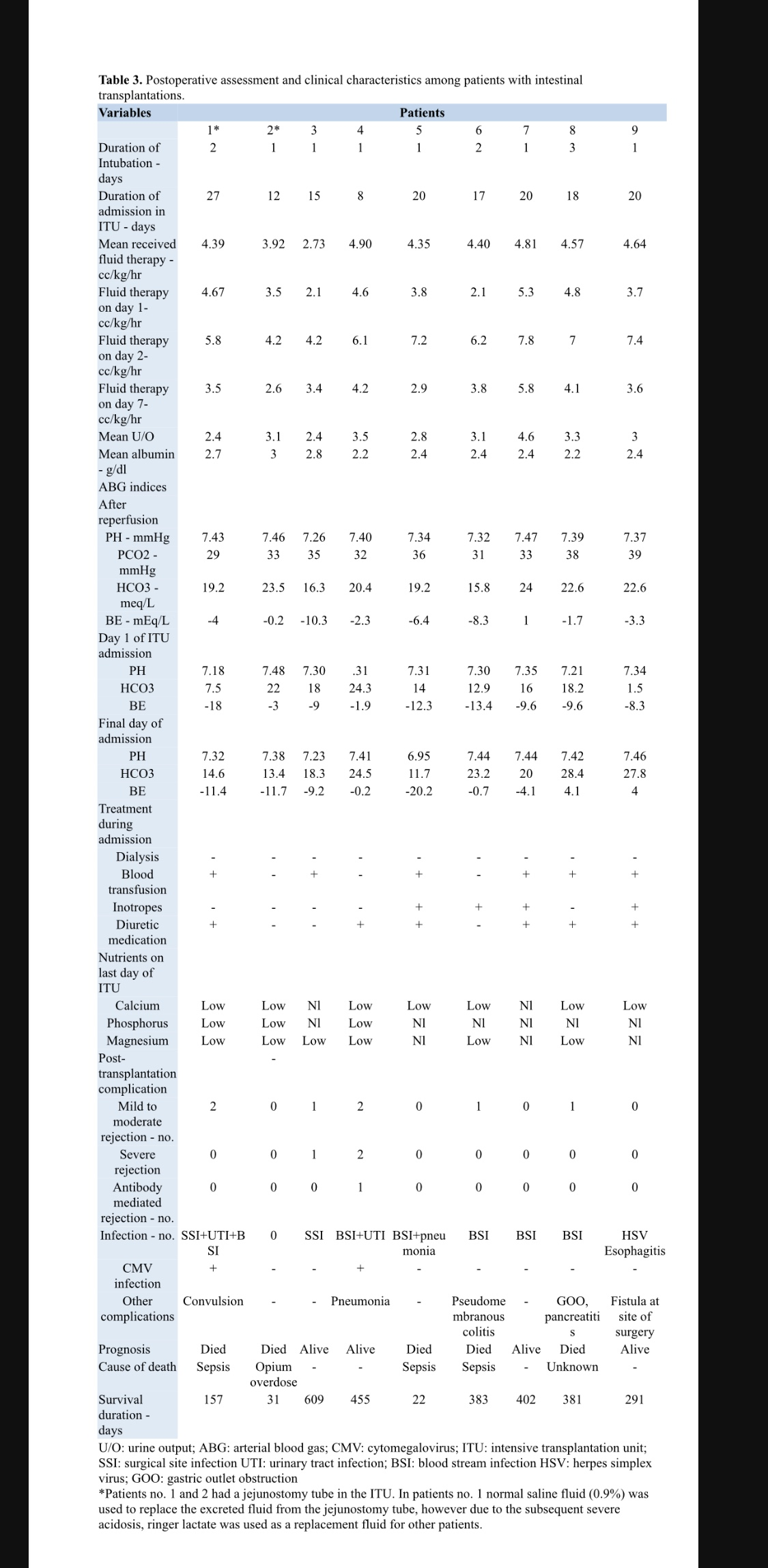
Results: Mean (SD) age of patients was 37.5 ± 12.5 years. Majority of patients were females (7/9). Median (IQR) waiting time for patients from diagnosis to transplantation 79 (34, 164) days. Our seven day survey of the amount of fluid therapy after transplantation, revealed that the greatest need for fluid therapy was seen on the second postoperative day. After transplantation two patients showed a total of three episodes of severe rejection, one of which was antibody mediated. The one-year survival was 66.6% and the two year survival was 44.5% in our study population. The median (IQR) time to death was 157 (26.5, 382) days. Most common cause of death was sepsis in our series (3/5).
Conclusion: Acceptable outcomes can be obtained with ITx in countries without HPN by application of specific treatment protocols.
Keywords: Intestine; Transplantation; Parenteral nutrition; Anesthesia; Fluid therapy; Autologous gastrointestinal reconstruction.