Decreasing therapeutic anticoagulation and bleeding in post-operative liver transplant patients: a single institution’s analysis of a prospective anticoagulation algorithm
Alexandria Tran1, Jorge Sanchez-Garcia2, Fidel Lopez-Verdugo2, Spencer LecorChick2, Richard K Gilroy3, Ivan Zendejas2, Manuel Rodriguez-Davalos2, Scott M Stevens4,5, Scott C Woller4,5, Diane Alonso1.
1Department of General Surgery, University of Utah Hospital, Salt Lake City, UT, United States; 2Transplant Service, Intermountain Medical Center, Murray, UT, United States; 3Hepatology Service, Intermountain Medical Center, Murray, UT, United States; 4Thrombosis Clinic, Intermountain Medical Center, Murray, UT, United States; 5Department of Internal Medicine, University of Utah School of Medicine, Salt Lake City, UT, United States
Introduction: The incidence of venous thromboembolism (VTE) in patients after liver transplantation (LT) is 0.4% to 15.5%. Management in the acute post-operative setting is challenging given the increased risk of bleeding. The aim of this study was to evaluate the implementation of a standardized VTE risk stratification algorithm to safely decrease the unnecessary implementation of therapeutic anticoagulation.
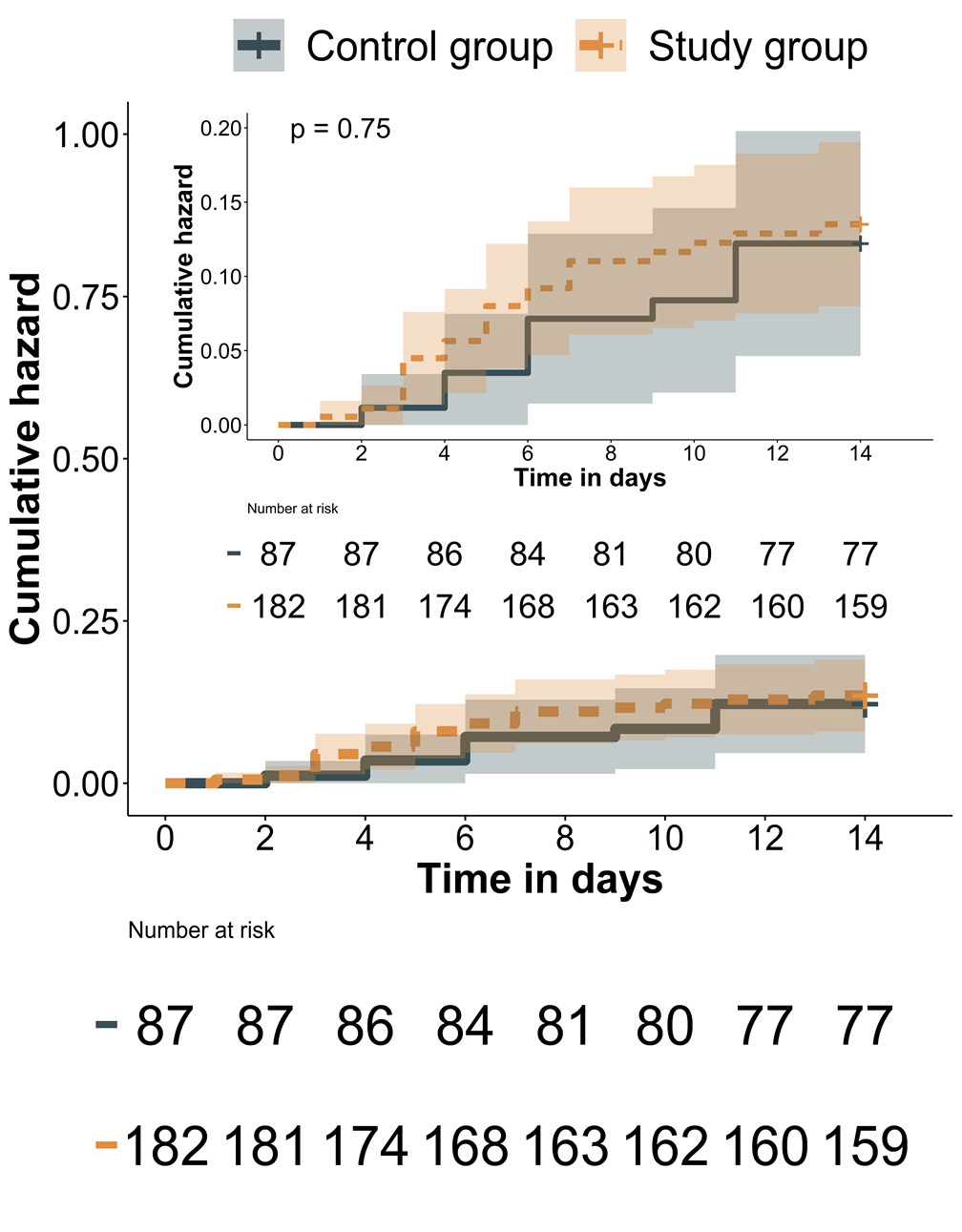
Methods: 87 (January 2016 - December 2017) and 182 LT patients (January 2018 - March 2021) were enrolled before and after the implementation of the algorithm, respectively. Primary endpoints included therapeutic anticoagulation for the treatment of a VTE within 14 days after LT and clinically significant bleeding. Safety outcomes included return to the operating room for bleeding, readmission, pulmonary embolism (PE), or death within 30 days after LT.
Results: Demographics were similar between groups. Following LT, 23 and 10 patients developed a VTE in the study and control groups, respectively. MELD score (OR = 1.06, 95% CI: 1.01-1.11; p=0.01) and number of operative lines (OR =1.35, 95% CI: 1.03-1.78; p=0.033) were associated with VTE development. Length of stay was longer among patients who developed a VTE (14 vs 10 days, p<0.001). The study group had decreased odds of receiving immediate anticoagulation (OR= 0.12, 95% CI: 0.019-0.587; p= 0.013) and of clinically significant bleeding (OR= 0.14, 95% CI: 0.02-0.91; p= 0.048). PE (p=0.8); re-operation (p=0.8), readmission (p=1), and death (p=0.8) were similar between groups.
Conclusions: This risk stratified VTE treatment algorithm in LT patients safely decreased rates of post-operative therapeutic anticoagulation and of clinically significant bleeding without an increase in early adverse outcomes.