Reno-portal anastomosis in liver transplantation with complex portal vein thrombosis. Results of a single center experience in Mexico
Paulina Carpinteyro-Espin1, Alejandra Ingle-González1, Karen Monroy-Rodriguez1, Alejandra Garcia-Anzurez1, Nayelli C Flores-Garcia1, Rodrigo Cruz-Martinez1, Mario Vilatoba1.
1Department of Transplantation, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, , Mexico
Introduction: Portal vein thrombosis has been reported in liver cirrhosis (1-28%) and is not an uncommon scenario in patients in the waiting list for a liver transplant. Portal inflow is extremely important for successful revascularization of the liver graft and resolution of portal hypertension. Complex portal vein thrombosis represents a challenge in liver transplant surgery. Reno-portal anastomosis, first described in 1997, is a technique used in selected patients for portal reconstruction in complex portal vein thrombosis with splenorenal shunt, however it is not extensively reported (around 66 cases in total). The aim of this study is to describe and analyze the outcomes of patients with a reno-portal anastomosis at our institution.
Method: We reviewed patients that underwent liver transplantation at our institution, from 2018 to 2021. Those who underwent reno-portal anastomosis were included. Descriptive analysis was performed. Variables were extracted from our prospective database and analyzed with SPSS Version 22.0.
Results: Of 168 liver transplants, 7 allografts (4.2%) were primarily revascularized with a reno-portal anastomosis. All of them had portal thrombosis Yerdel IV and a significant spleno-renal shunt detected preoperatively with CT. 6 patients (85.7%) were male. The median age was 49 (30-66) years and median BMI was 27 (22-34.2). Table 1 summarizes the more important variables studied.
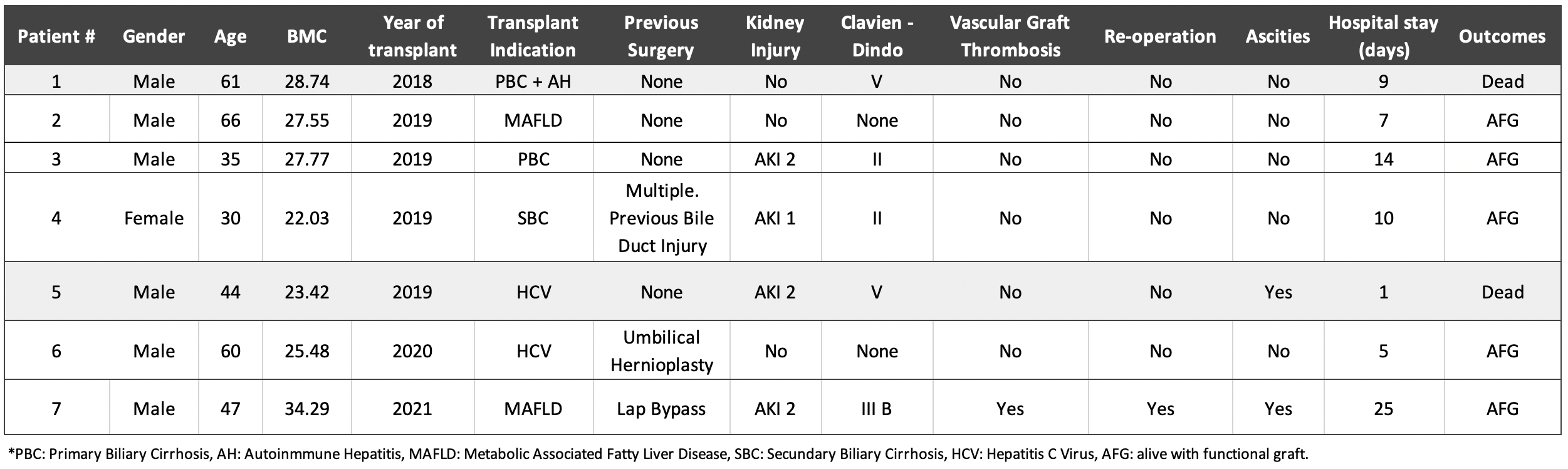
Complications were present in 5 patients (71.4%). Major complications (Clavien-Dindo > o = 3) were present in 3 patients (42.8%). 4 patients (57.1%) developed acute kidney injury however, all of them resolved within the first 48 hours and did not require hemodialysis. 2 patients (28.6%) developed ascites postoperatively, in one the portal reconstruction was thrombosed and in the other the portal inflow was not adequate. Only one patient (14.3%) presented vascular graft thrombosis and required reintervention. 2 patients (28.6%) died within 90 days: one of them despite reno-portal anastomosis did not presented adequate portal influx, the other died of pneumonia with a functional graft. The remaining 5 patients (71.4%) are alive with patent reno-portal anastomosis and normal liver function. The median follow up was 25 months.
Conclusion: Reno-portal anastomosis is a feasible option in patients with complex portal vein thrombosis and the presence of a significant spleno-renal shunt, achieving in most cases an adequate portal influx and resolution of portal hypertension, with low rate of thrombosis of the reconstruction. Our institute performs the largest number of liver transplants in Mexico. We experienced an evolution through the years, increasing our capacity to do more complicated procedures with acceptable results.
