Lung donors after circulatory death: an alternative of low technical difficulty that may potentially increase transplant-eligible lung availability
Nicolas Tommasino1, Raul Mizraji1, Mario Godino1.
1Departamento de Procuración, Instituto Nacional de Donación y Trasplante Uruguay, Montevideo, Uruguay
Introduction: Donor shortage is the main hindrance for achieving full development of Lung Transplant Programs. Donation after circulatory death (DCD), not yet widely used in Latin America, is a potential supply alternative to increase the availability of organs. The DCD Lung Donation Program designed for Uruguay is presented here.
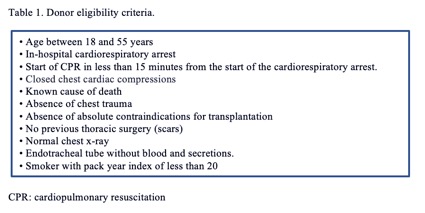
Method: To establish such type of a program, it is deemed necessary to have: a National Transplant Organization, appropriate legislation, an approved ethical framework and specialized teams of professionals. In Uruguay, organ donation and transplantation is governed by the National Institute of Donation and Transplantation (INDT). Under Law 14005, organs are allowed to be used for therapeutic purposes once irreversible pathological changes deemed incompatible with life are confirmed. The Ethics Committee has agreed that the treating physicians (independent from INDT) are those responsible for confirming the patient’s decease upon a cardiac arrest, and once CPR procedures have proved unsuccessful. Upon confirmation of patient’s decease, DCD lung donation is considered. INDT is called in, being responsible for donor selection (Table 1) and conducting the legal procedures. 500 units/kg of heparin are administered plus 10 cycles of closed cardiac massages. 300 cc of venous blood are then extracted, which are stored in a transfusion blood bag. Samples are taken for serology purposes, routinary procedures and chest x-ray performed. Chest tube placement in each hemithorax, second intercostal space, clavicular middle line. Maximum time between the cardiorespiratory arrest start and tube placement: 120 minutes. 6 litres of Perfadex® preservation solution or cool normal saline at 4 ºC is then introduced in each hemithorax. Next, Ventilator is switched-off. This way, the collapsed lung is maintained cool in a preservation solution until lung is removed in the operating room. Maximum time between topical preservation starts and lung removal begins: 240 minutes. Inside the operating room, drainage of both hemithorax is conducted. Ventilation starts at FIO2 100% and 5-cm H2O PEEP. Bronchoscopy is performed if needed. Cannulation of pulmonary artery and drainage of left auricle. Lavage is performed until clear liquid is obtained. Infusion through pulmonary artery of venous blood previously extracted with E2 prostaglandin. Blood gas is then extracted at the entrance, through the pulmonary artery and the affluent of each of the lung veins. If PaO2 difference between both samples is > 300 mmHg, then these are transplant-eligible lungs. Organ procurement and preservation is done through normal procedure.
Results: Protocol is approved by INDT and Ethics Committee. Its implementation has been delayed due to COVID pandemic.
Conclusion: These DCD programs do not imply technical complexities, but they do involve organization and procurement challenges. They are an alternative to increase the number of organs suitable for transplantation.