
Differences in short-term and medium-term prognosis between female and male heart transplant recipients: analysis of more than 20 years in a single center in Argentina
Elian F. Giordanino1, Daniel O. Absi1, Maria F. Renedo1, Liliana E. Favaloro1, Mariano Candiotti1, Rosario Della Cella Figueredo1, Carolina Putaro1, Roberto R. Favaloro1, Alejandro M. Bertolotti1.
1Heart failure, mechanical circulatory support and heart transplantation, Favaloro Foundation University Hospital, Ciudad Autonoma de Buenos Aires, Argentina
Introduction: There are differences in the clinical course of advanced heart failure between men and women. In addition, it has been reported that the prognosis after heart transplantation may differ according to the gender of the recipient, with different results in the literature.
The objective of this study is to characterize the demographic and clinical differences between male and female recipients in our population, as well as to analyze their short- and medium-term outcomes.
Method: Heart transplant recipients between February 1993 and February 2016 were retrospectively evaluated. Those with a follow-up of less than 5 years were excluded. Male and female recipients were compared and differences in short- and medium-term prognosis were analyzed. Quantitative variables are expressed as mean +/- standard deviation or median and interquartile range 25-75 according to their Gaussian distribution, and categorical variables as percentages. T-test or Mann-Whitney test was used to compare quantitative variables according to their normal distribution, and Fisher's test to compare nominal variables. Survival at 5 years was analyzed using the log-rank test and plotted using Kaplan-Meier. Univariate analysis was performed and variables with a p<0.2 were used for multivariate analysis using Cox regression. A p<0.05 was considered significant
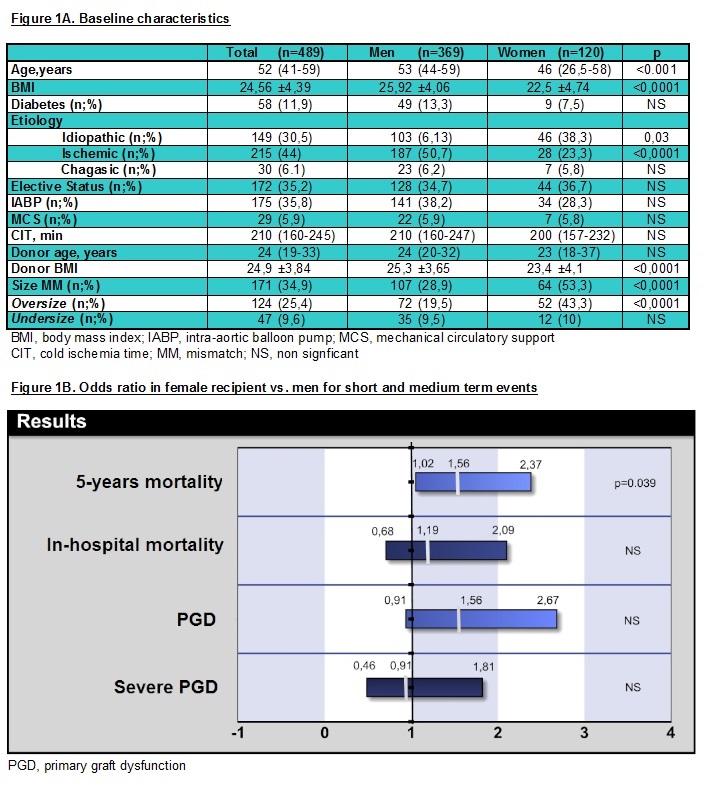
Results: Overall, 489 patients were included, 369 men (75.5%) and 120 women (24.5%). The characteristics of the population are shown in Figure 1A. The median age was 52 years (IQR 41-59), with the women being younger and with a lower body mass index (BMI). Regarding the etiology, idiopathic cardiomyopathy was more frequent in women and ischemic cardiomyopathy in men. There were no differences in elective status, level of hemodynamic support, or pre-transplant ischemia times. Although the women received donors with lower BMI, the size mismatch was greater in this group at the expense of greater oversize. The incidence of primary graft dysfunction (PGD), severe PGD, and in-hospital mortality was similar between men and women, however, female recipients had higher 5-year mortality (34.4% vs. 45% OR 1.56; CI 1.03 -2.37; p=0.039), without differences in the causes of death (Figures 1B and 2). In the multivariate analysis, female recipient, PGD and emergency condition were independent predictors of 5-year mortality. When analyzing the subgroup of female recipients, PGD and size mismatch at the expense of oversize were associated with higher mortality, however, in the multivariate analysis, only PGD maintained statistical significance. (HR 2.45, CI 1.19-4.26, p= 0.013) (Figure 3)
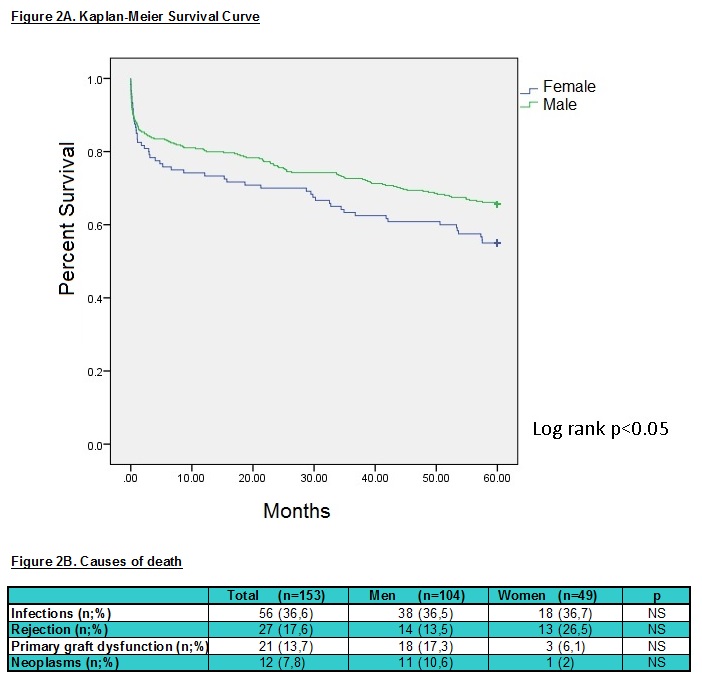
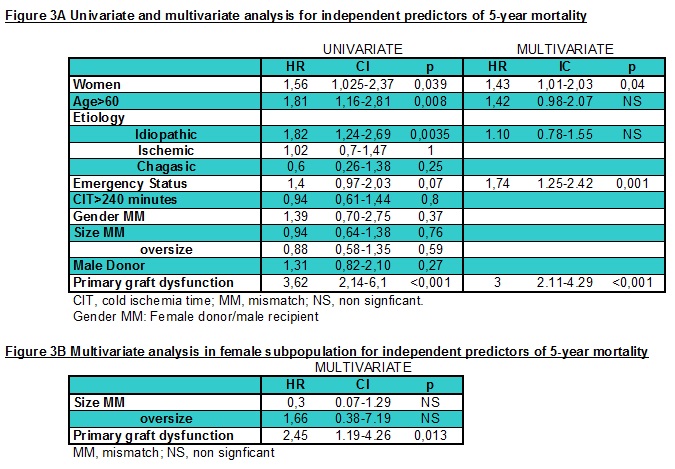
Conclusion: Female heart transplant recipients have a worse prognosis in the medium term with higher mortality at 5 years, without differences in hospital mortality. Larger studies are required to elucidate the underlying mechanisms with their potential therapeutic implications.

right-click to download
