
COVID-19 associated fungal co-infections in solid organ transplant recipients: a single center case series
Akshay Khatri1, Jacques Simkins1,2, Neeraj Sinha2, Anita Phancao2, Gaetano Ciancio2, Lilian M. Abbo1,2, Giselle Guerra2, Yoichiro Natori1,2, Shweta Anjan1,2.
1Department of Medicine, Division of Infectious Disease, University of Miami Miller School of Medicine, MIAMI, FL, United States; 2Miami Transplant Institute, Jackson Health System, MIAMI, FL, United States
Introduction: During the ongoing Coronavirus disease 2019 (COVID-19) pandemic, there have been increasing reports of co-infections with viral, bacterial and fungal pathogens. Two specific COVID-19-related fungal infections have been identified – COVID-19 associated pulmonary aspergillosis (CAPA) and COVID-19 associated mucormycosis (CAM), with limited information available about their incidence and occurrence in solid organ transplant recipients (SOTRs). We describe our experience with COVID-19 associated fungal co-infections (CFIs) in SOTRs with COVID-19.
Methods: This was a single center retrospective study at a large volume transplant center in South Florida, USA. We included adult SOTRs (≥18 years) diagnosed with COVID-19 between March 1st 2020 and January 31st 2022, with a subsequent diagnosis of CFI. We collected information related to demographics, comorbidities, COVID-19 diagnosis and therapeutics, and CFI diagnostics and management. We performed descriptive statistical analysis on the data obtained.
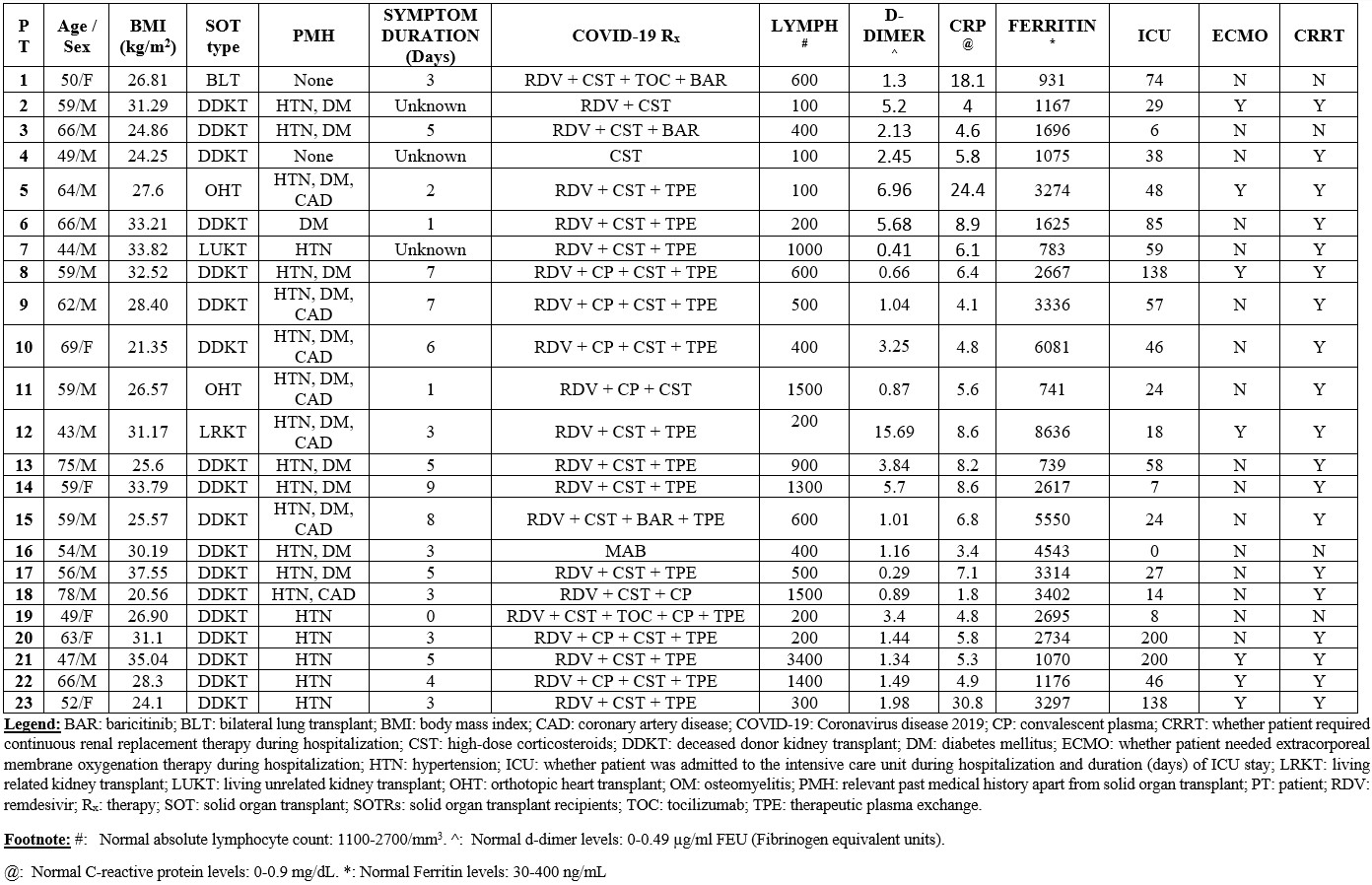
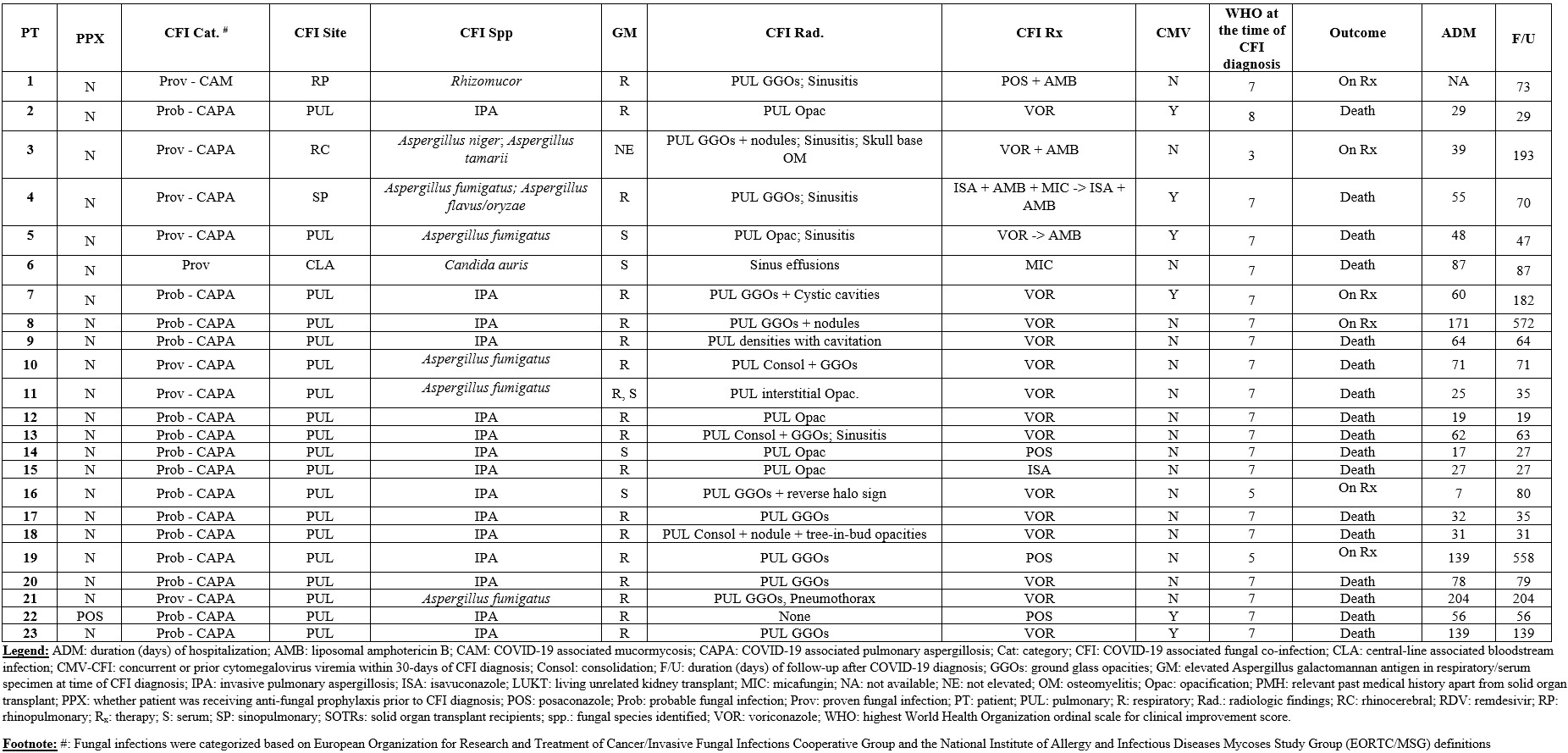
Results: We identified 612 SOTRs with COVID-19, of which 23 (3.8%) were diagnosed with CFIs. The patients were predominantly male (17/23, 73.9%), with median age of 59 years (range 43-79) (Table 1). Twenty (86.9%) were kidney transplant recipients. Majority of SOTRs had lymphopenia (18/23, 78.3%) with elevated inflammatory markers at time of COVID-19 diagnosis. They received most commonly remdesivir and corticosteroids for COVID-19, with 22 (95.6%) needing intensive care unit admission and 19 (82.6%) needing continuous renal replacement therapy. CFIs were diagnosed at median 21 days (range, 3-161) after initial COVID-19 diagnosis. Probable CAPA was diagnosed in most patients (16/23, 69.6%), with CAM noted in 1 patient (Table 2). 34.8% (8/23) had specific fungal species identified, with elevated fungal markers noted in 95.6% (22/23). Concurrent or prior cytomegalovirus DNAemia was noted in 26.1% (6/23). Patients were followed for median 70 days (range, 19-572), with median hospitalization duration 56 days (range, 7-204). Mortality was noted in 73.9% (17/23).
Conclusion: Fungal co-infections were noted in a small proportion of our SOTRs, with poor outcomes. Transplant physicians should have a high suspicion for early diagnosis and treatment of CFI. Further studies are needed to determine predictors for CFI and role for anti-fungal prophylaxis.

right-click to download
