Response to a pandemic: the fall and rise of kidney transplantation in the United States
Shivani Bisen1, Brian Boyarsky 1, William Werbel1, Jon Snyder1, Laura B. Zeiser1, Jacqueline Garonzik-Wang2, Macey L. Levan1, Dorry L. Segev1,3,4, Allan B. Massie1,3.
1Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, United States; 2University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; 3Department of Epidemiology, Johns Hopkins University School of Public Health, Baltimore, MD, United States; 4Scientific Registry of Transplant Recipients, Minneapolis, MN, United States
Epidemiology Research Group in Organ Transplantation.
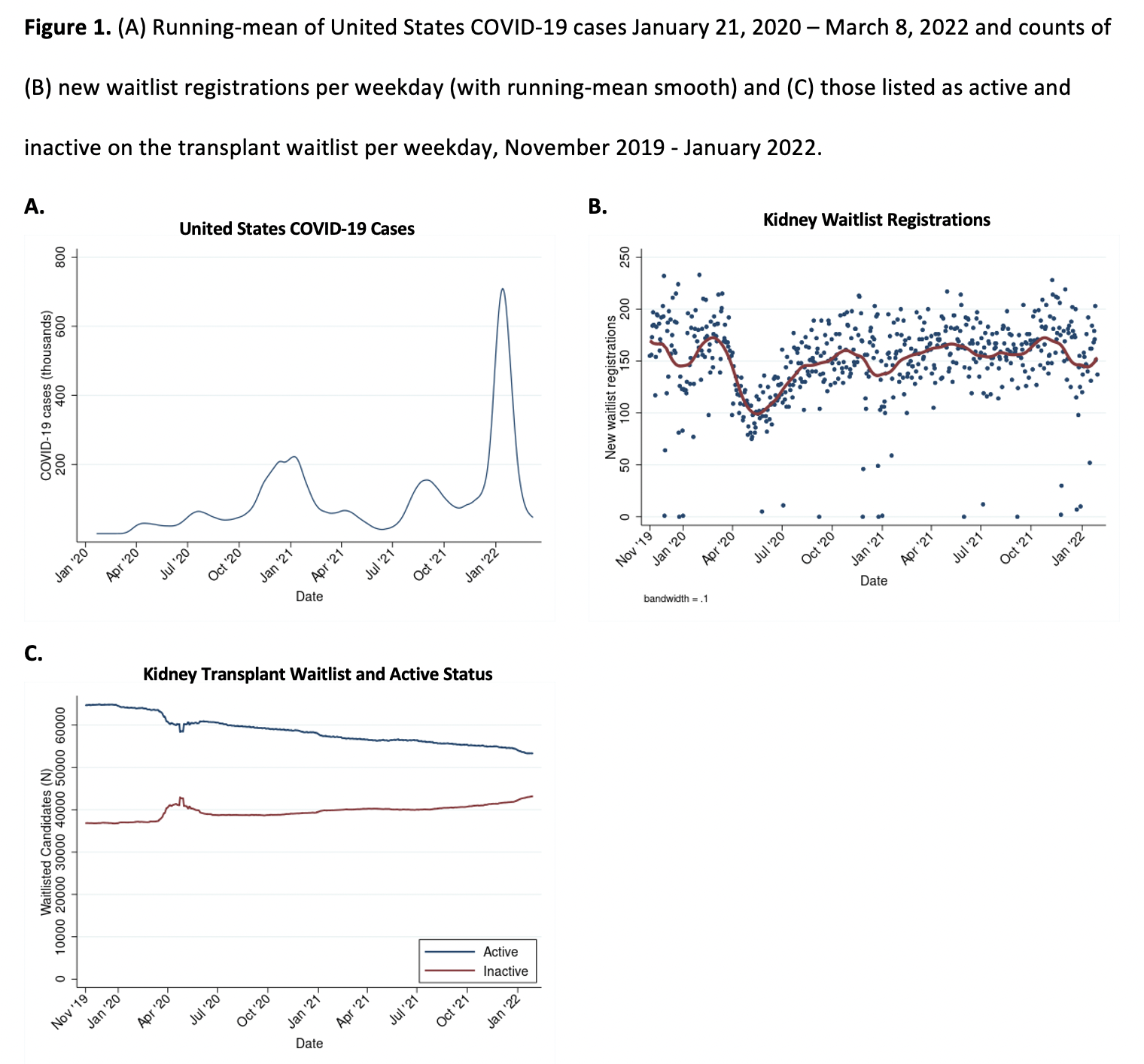
Background: Following the outbreak of COVID-19 in the United States, the number of kidney waitlist additions and living-donor and deceased-donor kidney transplants (LDKT/DDKT) decreased substantially but began recovering within a few months. Since then, there have been several additional waves of infection, most notably, the Delta and current Omicron surge beginning in August and December 2021, respectively. By 1/12/2022, the Omicron surge peaked at 802,699 confirmed new cases, compared to a pre-Omicron peak of 251,772 confirmed new cases on 1/8/2021, demonstrating an immense disease burden on the American population that could have been enough to disrupt transplant practices.
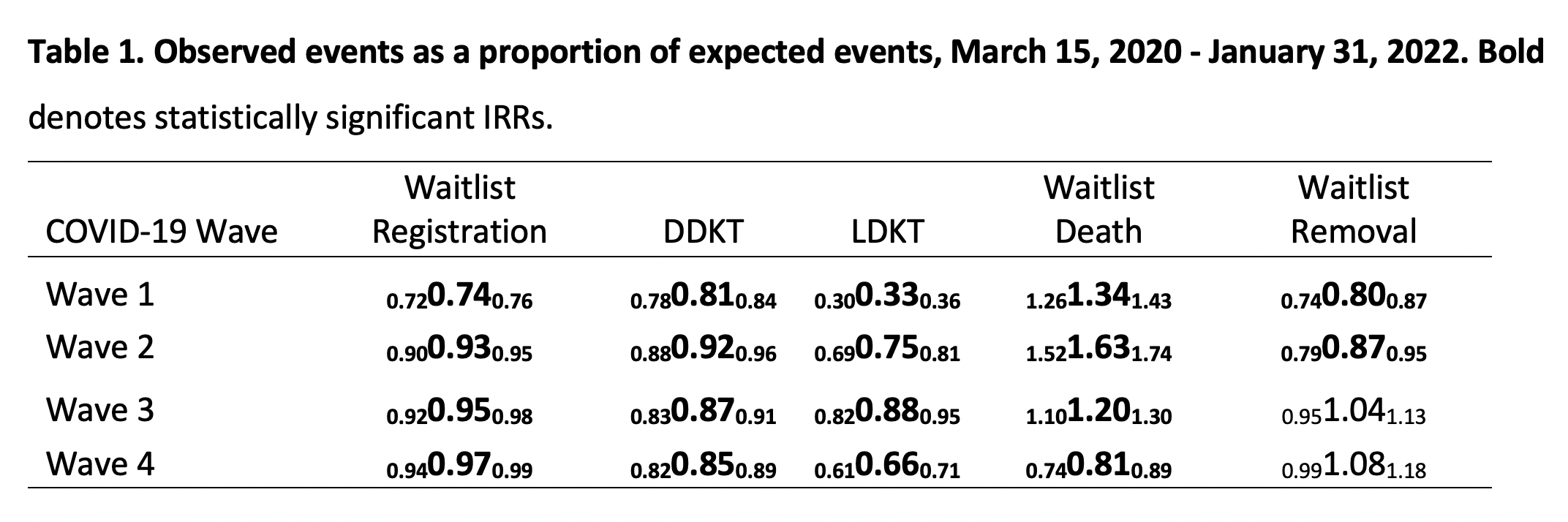
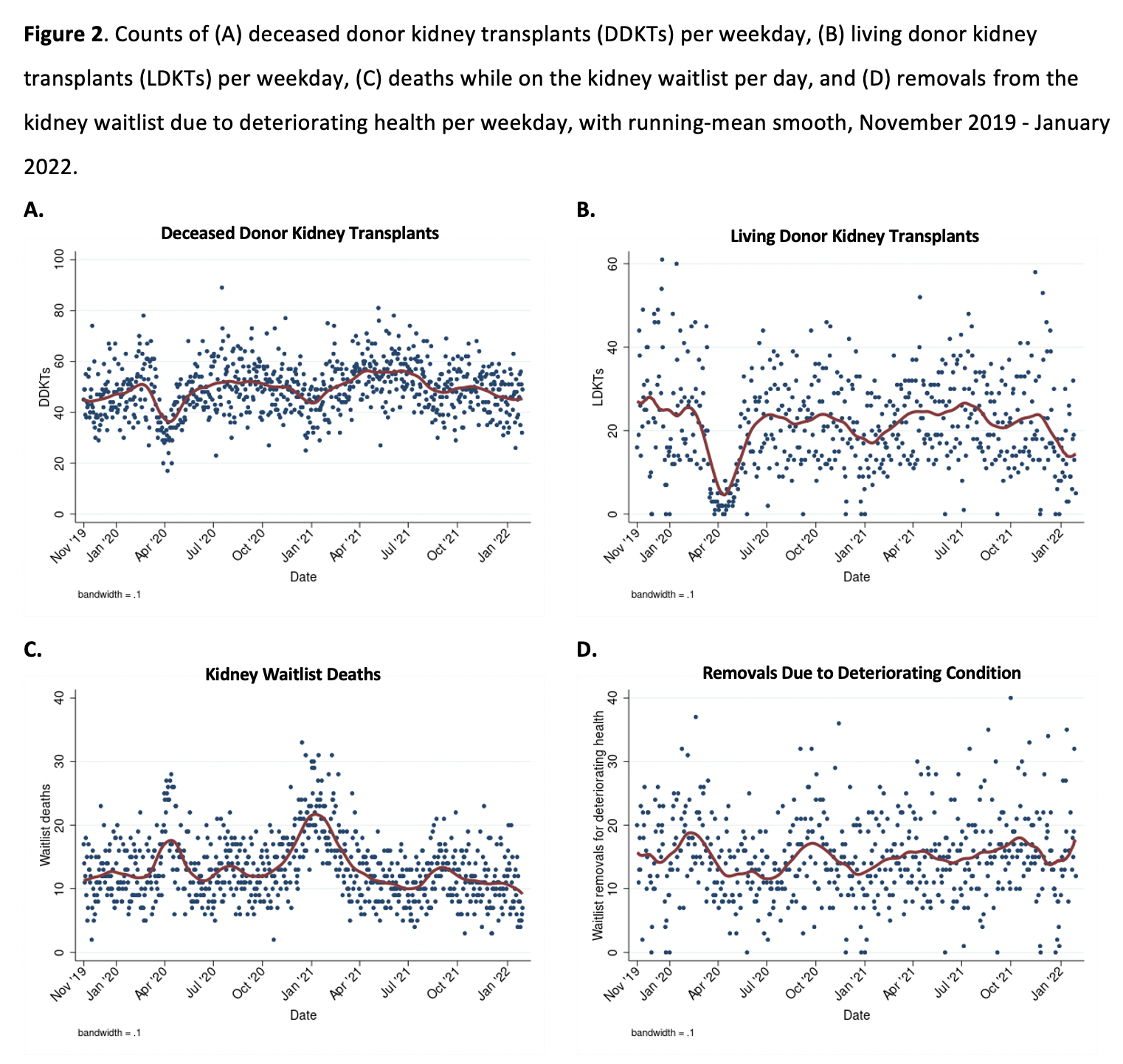
Methods: Using data from the Scientific Registry of Transplant Recipients (SRTR), we compared observed waitlist registrations, waitlist mortality, waitlist removal, LDKT, and DDKT in the United States over four distinct pandemic waves to expected events based on calculations from pre-epidemic and non-wave pandemic data, while accounting for seasonality and secular trends. Four distinct time periods/waves of high COVID-19 incidence in the United States were identified for analysis. Wave 1 was defined March 15, 2020 – May 31, 2020; Wave 2 was defined December 1, 2020 – January 31, 2021; Wave 3 was defined August 1, 2021 – September 30, 2021; and Wave 4 was defined December 1, 2021 – January 31, 2022. Waves 1, 2, 3, and 4 were referred to as the Initial, Winter 2021, Delta, and Omicron waves during our analysis.
Results: Although the number of daily waitlist additions has been increasing since May 2020, the size of the active waitlist has consistently declined, reaching a minimum of 53,180 on 1/31/2022. The recent Omicron surge knocked LDKT from 12% below expected (IRR = 0.820.880.95) during the Delta wave to 34% below expected (IRR = 0.610.660.71). DDKT, in contrast, was relatively unaffected by the Omicron wave (IRR = 0.830.870.91 and 0.820.850.89 during the Delta and Omicron waves, respectively). Waitlist death declined from 20% above expected (IRR = 1.111.201.30) during Delta to 19% below expected (IRR = 0.740.810.89) during Omicron, whereas waitlist removal remained at expected levels throughout both (IRR = 0.951.041.13 and 0.991.081.18 during Delta and Omicron, respectively). Note, this was the first time that an outcome returned to expected levels since the start of the pandemic.
Conclusions: The Omicron wave brought substantial declines in DDKT and LDKT that have not been seen since the Initial wave. Due to vaccine mandates in place at many transplant centers across the nation, the American SRTR population now has high levels of vaccination including high levels of second and third booster shots. Hence, despite the Omicron wave's exceptionally high COVID-19 infection incidence in the American national cohort, there was no increase in waitlist mortality, likely due to vaccination.
Ben‐Dov family. K24AI144954 from National Institute of Allergy and Infectious Diseases (NIAID). K01DK101677 from National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).

right-click to download
