Controlling instability at reperfusion: another benefit of normothermic machine perfusion using OCS liver
Christine Hwang1, Chen Shi2, Madhukar Patel1, Jigesh Shah1, Lucia de Gregorio1, Steven Hanish1, Yash Kadakia1, Usama Chaudhary1, Ejike Okoro2, Sreekanth Cheruku2, Peiman Lahsaei2, Parsia Vagefi1, Malcolm MacConmara1.
1Surgery, UT Southwestern Medical Center, Dallas, TX, United States; 2Anesthesia, UT Southwestern Medical Center, Dallas, TX, United States
Introduction: Organ Care System (OCS) Liver is a portable ex-vivo normothermic liver perfusion device recently shown to provide superior donor organ preservation. The impact of OCS Liver on post-reperfusion syndrome (PRS) remains unknown.
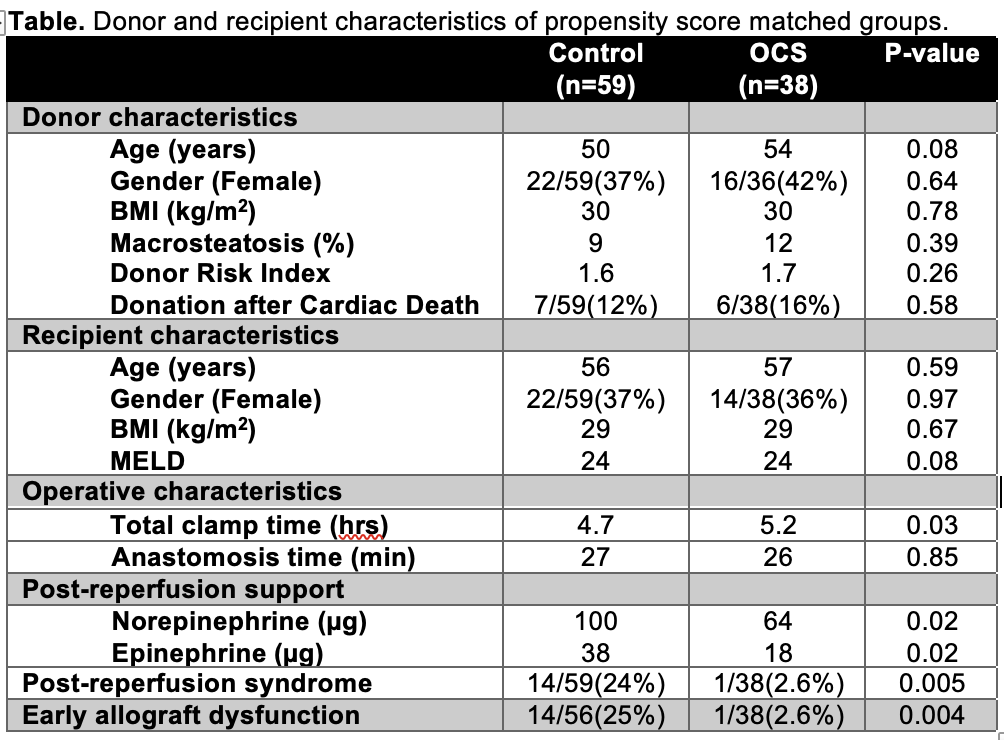
Method: This was a retrospective, single center, case-control study. All transplants utilizing OCS Liver between 1/1/2018 and 12/31/2020 were compared with a propensity score matched (PSM) cohort . The control population was matched for age, MELD, donor type and ventilator/circulatory support. Multiorgan transplants were excluded from the analysis. Donor, procurement, and recipient characteristics were collected for all recipients. Anesthesia records containing vitals by minute and pressor/inotropes were collected to establish baseline (5 minutes prior to reperfusion) and up to 30 minutes post-reperfusion hemodynamics.
Results: Following PSM there were 97 liver transplants in the study cohort, including 38 OCS (39%) and 59 controls (61%). Donor and recipient characteristics confirmed these groups were well matched. PRS, defined by ≥1 minute of mean arterial pressure 30% below baseline, was significantly reduced in the OCS group (1/38(3%) vs. 14/45(24%), p=0.005). OCS patients required significantly less post-reperfusion support, where both total norepinephrine (64 μg vs. 100 μg, p=0.02) and total epinephrine (18 μg vs. 38 μg, p=0.02) infusions were reduced compared to controls. Patients with combined blood pressure instability and pressor support were more likely to develop early allograft dysfunction (EAD), (15/56(27%) vs. 0/38(0%), p=0.001). However, the use of OCS was associated with a 10-fold reduction in EAD (1/38(2.6%) vs. 14/56(25%), p=0.004).
Conclusion: Normothermic machine perfusion using OCS Liver reduces hemodynamic instability after reperfusion and also results in a significantly reduced incidence of EAD.

right-click to download
