
Manuel Rodriguez-Davalos, MD, joins the University of Utah as the Living Donor Liver Transplant Program Director for the Division of Transplantation & Advanced Hepatobiliary Surgery. Dr. Rodriguez is also Section Chief of Abdominal Transplant and Director of Pediatric Liver Transplantation at Intermountain Primary Children’s Hospital.
A graduate of Universidad Anahuac in Mexico, his career in liver disease began in 1996 as a post-doctoral fellow at national institute of medical sciences in Mexico City. After 15 years working in adult and pediatric transplantation in the northeast coast of the United States, he left his position as Director of Pediatric Abdominal Transplantation at Yale, where he was an Associate Professor of Surgery and Pediatrics and moved to Utah to take the position of Surgical Director of Pediatric Liver Transplant.
His focus is liver disease with interest in living donor liver transplantation, as well as hepatic malignancies and portal hypertension. Dr. Rodriguez has worked with UNOS pediatric and liver-intestine committees as regional representative and member at large. Currently, he works with the national pediatric allocation task force, the registry committee, and the council of Society of Pediatric Liver Transplantation (SPLiT) and IPTA. He is an associate editor of the journal Transplantation. He is an active member of the North American Living Liver Donor Innovations group, ILTS Pediatrics committee past chair and TTS Education committee.
His current research is focused on the use of technology including advanced quantitative modeling techniques with 3D imaging and 3D printing. He investigates the use of split grafts and other extended criteria to decrease the mortality on patients on the liver transplantation waiting list. With the team at Primary Children’s Hospital, and the investigators from the U of Utah Department of Surgery and Pediatrics, he is conducting work on pediatric hepatic malignancies, innovative vascular techniques for children with portal hypertension, as well as collaborating with the NIH funded-Childhood Liver Disease Research and Education Network. He is also in charge of the transplantation intiative with the Center for Global Surgery with current funded projects in Asia and Latin America, which include the TTS/ILTS Paired center project.
How whole slide imaging and AI can improve organ transplants
Leonardo Aviles Ovalle1, Nicholas Baker1, Ben Cahoon2, Kim Olechovski2, Talia Baker1, Jeffrey Campsen1.
1Department of Surgery, University of Utah, Salt Lake City, UT, United States; 2Techcyte Inc., Orem, UT, United States
Introduction: As the advancement and implementation of technology in healthcare diagnostics continue, the full capabilities may not be fully realized. Research and development of artificial intelligence (AI) within the transplantation realm are primary examples. The expansion of whole slide imaging and AI in kidney and liver transplantation presents immense opportunities to address significant logistical concerns. This includes the quality of pathology reports, speed of organ offer acceptance, and minimizing ischemic time. Globally, there is a high demand for organs to compensate for the increasing diagnosis of comorbidities requiring transplantation. Unfortunately, the technical and logistical barriers of evaluating cadaveric donor organs in an emergent but precise manner prohibit efficient allocation. Organ allocation can be further refined and post-transplant outcomes improved by seeking solutions that will produce consistent, high-quality pathology reports, regardless of time or properly trained pathologists. The implementation of AI stands to address these issues by introducing machine learning in accurately reading donation biopsies.
Methods: In the case of kidney and liver transplantation, when a cadaveric donor becomes available, biopsies are acquired to assess the viability of organ transplantation. Under ideal circumstances, these biopsies are read by a specialized pathologist. But many times biopsies are read by any available pathologist. This results in sub-par, inconsistent, and frequently delayed pathology reports. The reliance upon these reports subject’s organ recipients to inconsistent results that will impact long-term outcomes. Once the slides are digitized an AI algorithm can be trained to provide a consistent, accurate organ donation-focused pathology report at any time of day.
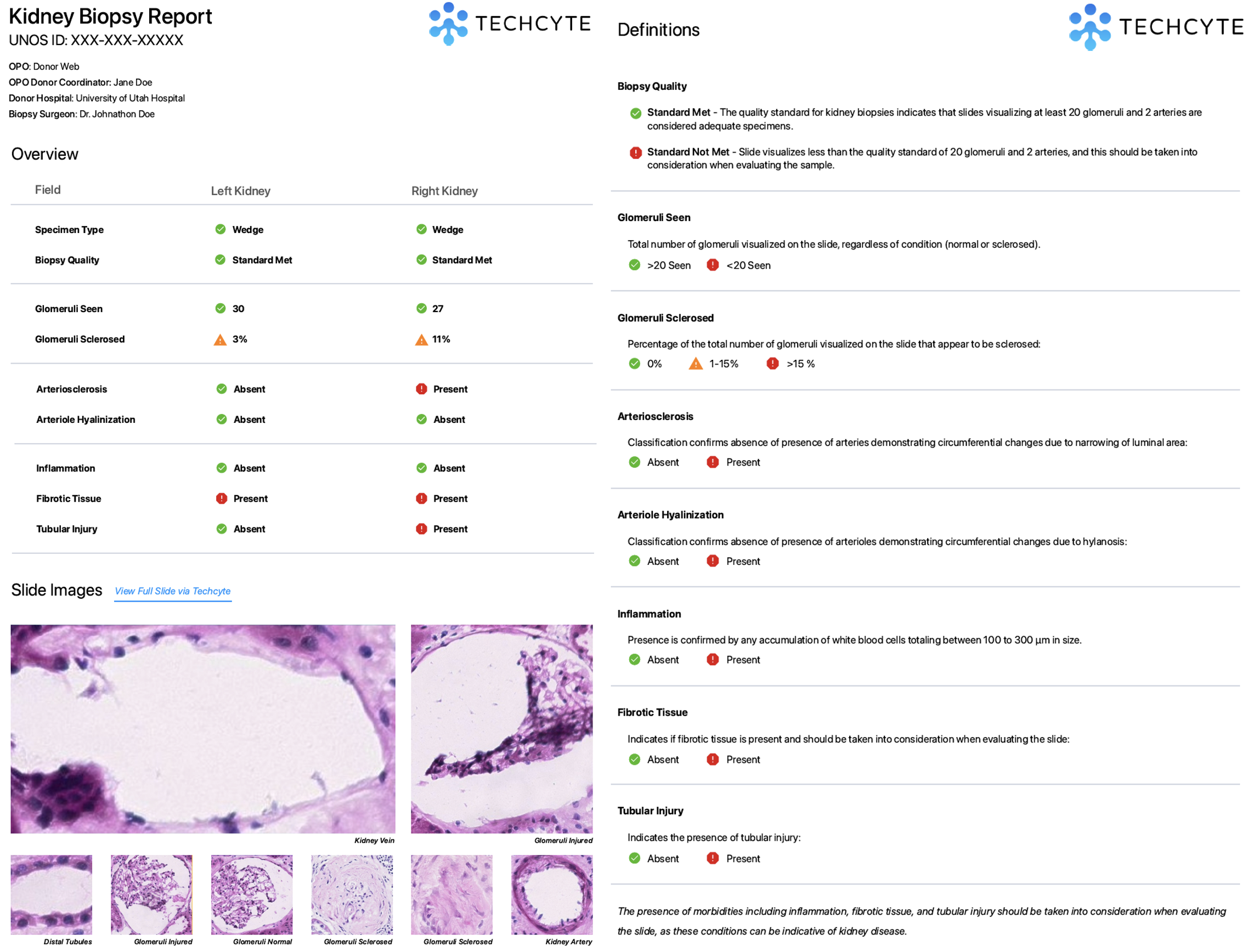
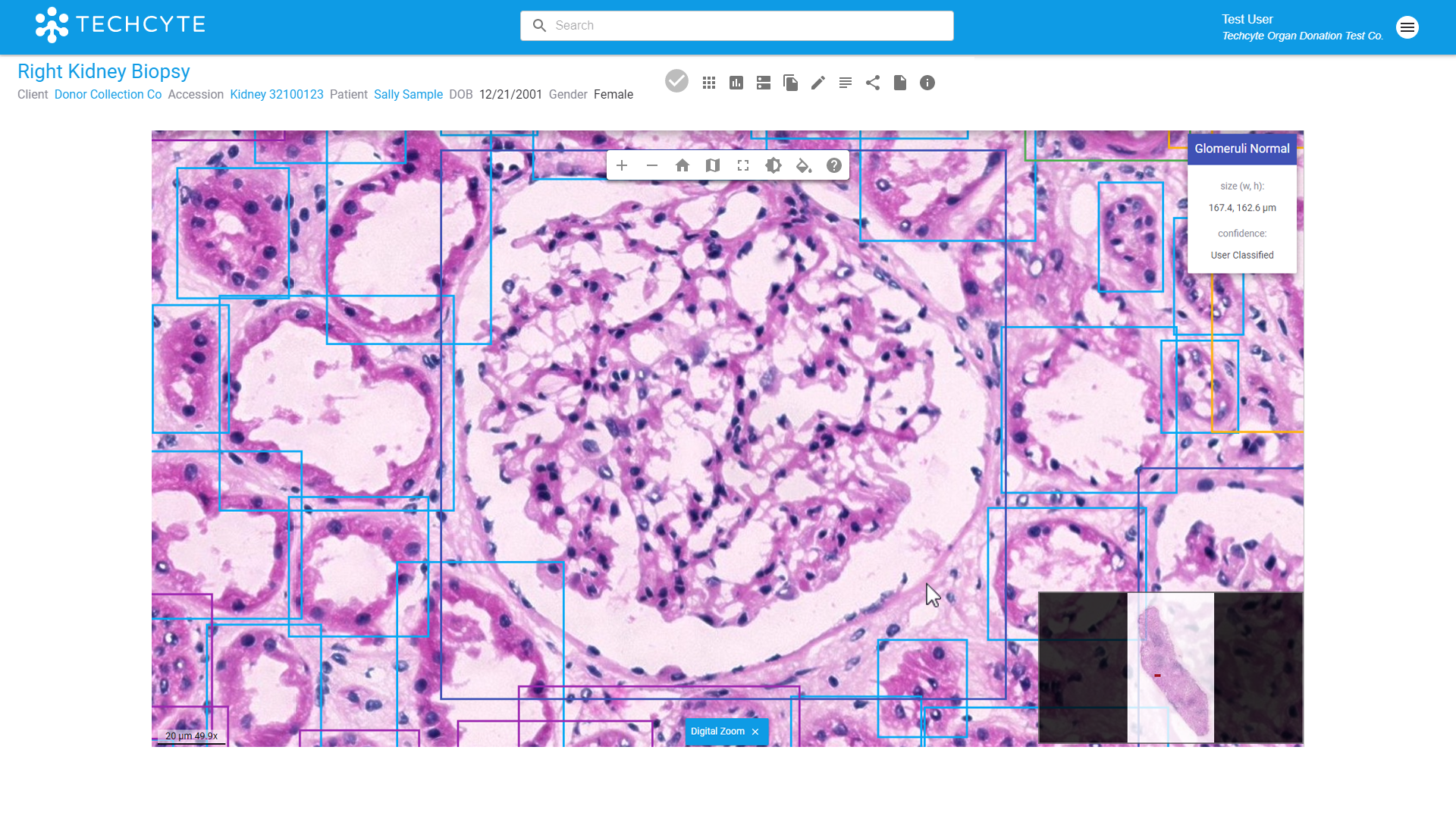
Conclusion: Whole slide imaging and AI can fill the gaps that negatively impact surgical decision-making and long-term patient outcomes. Technology that can improve the quality and accuracy of pre-transplantation biopsy reports, AI can significantly reduce the duration of getting organs to patients and avoid the transplantation of unviable organs. It can identify fibrosis and inflammation of the liver and kidney, sclerotic glomeruli, atrophied tubules in kidney samples, and large and small droplet macrosteatosis fat in liver samples. Increased efforts and resources to bolster the research and development of AI systems in transplantation can significantly benefit all parties involved in delivering high-quality care and positive long-term patient outcomes.

right-click to download
