
Evolution of thromboelastography parameters during pediatric liver transplantation
MIhaela Damian1, Daniel Tawfik 1, Julianne Mendoza2, Amy Gallo3, Carlos Esquivel 3.
1Pediatrics , Stanford University , Palo Alto , CA, United States; 2Anesthesia , Stanford University , Palo Alto, CA, United States; 3Surgery , Stanford University , Palo Alto, CA, United States; 4Pediatrics , Stanford University , Palo Alto, CA, United States
Background: Liver failure is characterized by abnormal bleeding and clotting as the liver produces the majority of procoagulant, fibrinolytic, and regulatory proteins of the coagulation system. Liver transplantation (LT) carries high risk of intraoperative bleeding. Thromboelastography (TEG), a global coagulation assay, measures several aspects of clot formation in real time and is used to guide blood product administration including LT. However, no data on description of TEG parameters during pediatric LT exist.
Methods: An IRB-approved retrospective review of subjects under 18 years of age undergoing LT between 2015 and 2017 was performed to describe the TEG parameters that were obtained at three time points (baseline, anhepatic and reperfusion) during LT and to evaluate blood product utilization during and immediately post-operation. Friedman Test to compare TEG parameters at the 3 timepoints, and Pearson correlation coefficients to evaluate association with blood product transfusion volumes were used.
Results: Demographic, clinical, surgical and post-surgical characteristics of 80 children that underwent LT are shown in Table 1. 39 subjects were females (49%). The majority had intrinsic liver disease 59 (74%). Two episodes of portal vein thrombosis occurred. Six subjects returned to the OR for postsurgical bleeding.
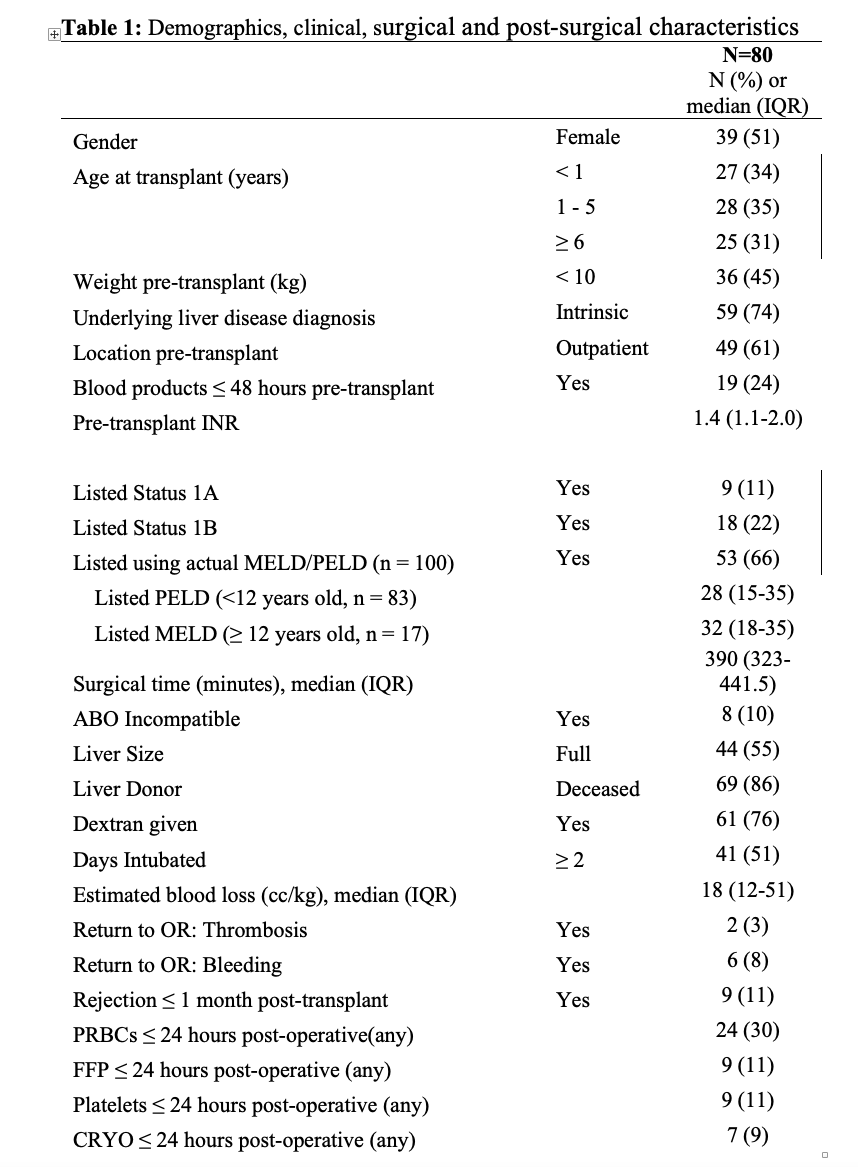
Figure 1 describe the TEG values for all 3 points during transplantation: All TEG parameters showed statistically significant change across the timepoints, although those obtained during anhepatic and reperfusion times were similar: median (IQR) maximal amplitude (MA) 57.8 (50.3-64.4) vs 53.3(44.3 -61.4) vs 53.8 (46.1-59.5), Alpha Angle (a) 67.9 (60.6-72.1) vs 61.4(48.5-69.5) vs 60.2 (47.9-67.8) and Citrate Kaolin (CK) R 5.2 (4.4-7.0) vs 6.2 (4.8-8.2) vs 7.1(5.6-9.0). MA and a decreased throughout the case while CK R time increased.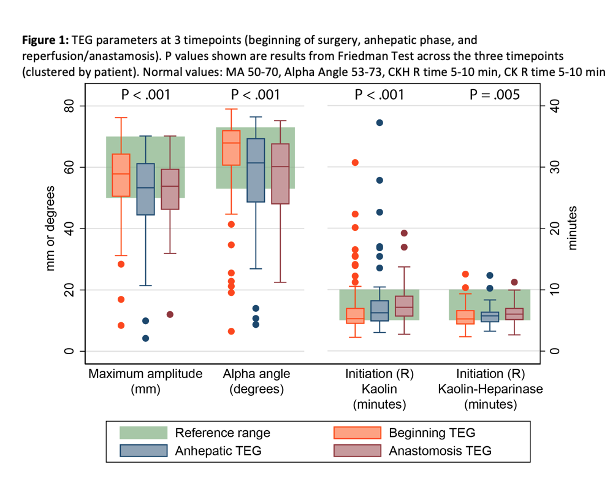
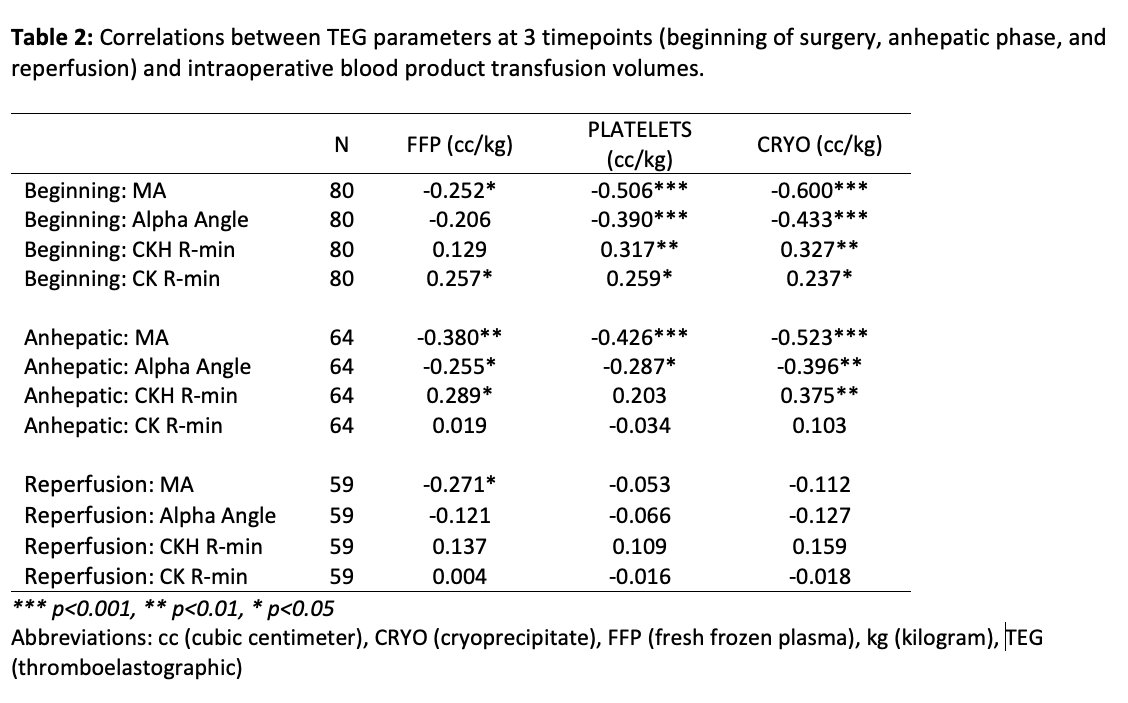
Summary characteristics of TEG results and correlates with intraoperative blood product transfusion volumes (Median (IQR) cc/kg body weight) are shown in Tables 2. 50 subjects (62%) received 20.8 cc/kg (10.2-34.1) fresh plasma, 36 subjects (45%) received 5.8 cc/kg (2.9 -8.7) cryoprecipitate and 29 subjects (36%) received 8.5 cc/kg (5.4-16.1) platelets. Intraoperative transfusion of any blood product correlated with nearly all baseline TEG parameters, and with anhepatic MA and alpha angle. Plasma transfusion correlated with MA at the reperfusion time.
Conclusions: This is the first descriptive analysis of TEG parameters during pediatric LT. During the surgical procedure there is transition from a hypercoagulable state to a longer time to form the blood clot and fibrinolysis. Intraoperative TEG guidance may allow more targeted support of coagulation using better transfusion algorithms without leading to more complications. Further studies to assess the adoption of TEG during LT need to be independently evaluated along with the establishment of meaningful outcome measures.

right-click to download
