ASCENT (allocation system changes for equity in kidney transplantation) implementation of randomized effectiveness study increased access to kidney transplant waitlist for black patients on dialysis
Rachel Patzer1,2, Jade Buford1, Megan Urbanski2, Hana Lee2, Adam Wilk1, Stephen O. Pastan2.
1Rollins School of Public Health, Emory University, Atlanta, GA, United States; 2School of Medicine, Emory University, Atlanta, GA, United States
Background: Black vs. white patients have longer time on dialysis and lower rates of kidney transplant access. The U.S. kidney allocation system (KAS) was overhauled in December 2014; however, no formal education was provided to dialysis facilities about the policy and its implications, including how patients with longer time on dialysis could get transplanted faster under the new system.
Methods: The ASCENT study was a cluster-randomized, pragmatic, multi-level (provider and patient), multicomponent educational and quality improvement effectiveness-implementation intervention intended to provide education and awareness of the KAS policy change among U.S. dialysis facilities with low waitlisting. A total of 655 U.S. dialysis facilities (>20,000 patients) were randomized. Intervention activities included an educational webinar for medical directors, a staff educational video describing KAS, a transplant performance audit and feedback report detailing the facility-specific impact of KAS, and a patient educational video; the control group received a brochure. Co-primary outcomes of the trial included dialysis facility-level 1-year waitlisting and racial disparity in waitlisting. Generalized linear models reported effects among incident and prevalent patients, adjusting for time trends and clustering of patients within facilities.
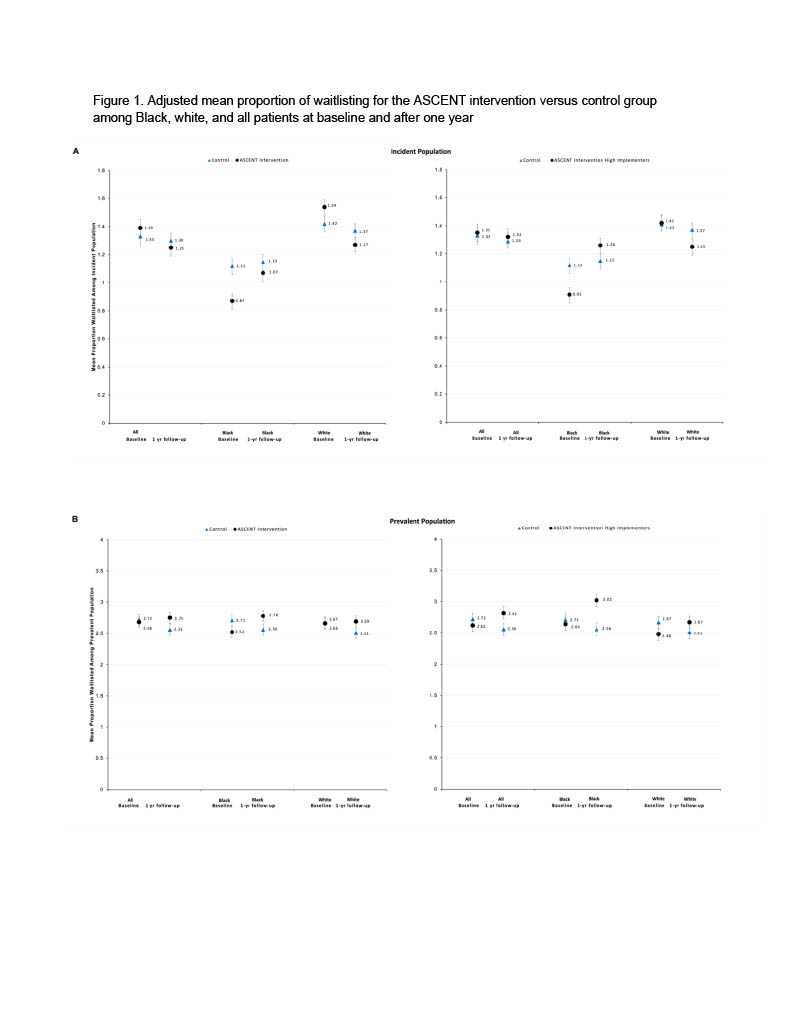
Results: Similar to national trends, the overall mean proportion of patients waitlisted in a facility declined 1 year after the intervention among incident patients (Figure, Panel A, left) in both the intervention vs. control facilities, and waitlisting was the same among prevalent patients (Figure 1, Panel B, left). However, the proportion of patients waitlisted declined for white ESKD patients in the intervention groups but increased for Black ESKD patients in both the incident (Figure 1, Panel A) and prevalent (Figure 1, Panel B) populations. Mean waitlisting significantly (p<0.05) increased among prevalent Black ESKD patients in the intervention group (baseline waitlisting: 2.52% (2.43, 2.61); follow-up: 2.78% (2.69, 2.87) while it declined among Black patients in the control group (baseline waitlisting: 2.71% (2.62, 2.80); follow-up: 2.56% (95% CI: 2.47, 2.65). In generalized linear models, overall differences in the mean proportion of patients waitlisted between intervention and control among Black patients at 12 months was 0.22% (0.02, 0.42), p<0.05. Among white patients, waitlisting declined in the control group and remained the same among intervention group facilities. Results were more pronounced among the 57% of intervention facilities considered high implementers (Figure 1, right).
Conclusions: The ASCENT educational and outreach intervention helped to extend the reach of this policy among U.S. dialysis facilities with low waitlisting in the population of prevalent Black patients who are most likely to benefit from the policy change.
This work was supported by a grant from the NIMHD: R01MD010290.

right-click to download
