Rates of effective intent-to-donate in Nova Scotia: mitigation of differences by gender and age after enactment of deemed consent legislation
Ethan Pancer1, Stephen Beed2,3, Karthik Tennankore4, Matthew J Weiss5,6, Kristina Krmpotic2,3.
1Sobey School of Business, Saint Mary's University, Halifax, NS, Canada; 2Department of Critical Care, Dalhousie University, Halifax, NS, Canada; 3Legacy of Life and Critical Care Organ Donation, Nova Scotia Health, Halifax, NS, Canada; 4Department of Medicine, Dalhousie University, Halifax, NS, Canada; 5CHU de Québec-Université Laval Research Center, Université Laval, Quebec, QC, Canada; 6Transplant Québec, Montreal, QC, Canada
LEADDR Program.
Introduction: Some of the highest rates of deceased donation activity in the world are observed in European countries with deemed consent legislation.(1) On January 18, 2021, Nova Scotia became the first jurisdiction in North America to implement a deemed consent model with the enactment of Human Organ and Tissue Donation Act (HOTDA). This study aimed to establish rates of effective intent-to-donate before and after enactment of deemed consent legislation in Nova Scotia.
Method: Analysis of aggregate data obtained from the Nova Scotia Organ and Tissue Donation Registry. The effective intent-to-donate (%) was determined as either the proportion of eligible Nova Scotians registering an opt-in decision pre-HOTDA or the proportion of eligible Nova Scotians registering an opt-in decision or not registering an opt-out decision post-HOTDA (January 18, 2021). Donor registration data was available from April 2018 (34 months pre-HOTDA) to February 2022 (12 months post-HOTDA). This data included a demographic breakdown by gender and age ranges (19-29, 30-48, 49-64, 65+) of eligible Nova Scotians.
Results: Rates of effective intent-to-donate increased from 49.0% to 51.9% in the 34 months leading up to HOTDA enactment, and from 51.9% to 99.1% in the month of enactment (Figure 1). In the 12 months post-HOTDA, rates of opt-out increased by 0.3% to 0.5% per month resulting in an effective intent-to-donate rate of 94.4% one year following enactment. At enactment, more females than males had registered an opt-in decision (54.7% vs. 49.1%). One year following enactment, rates of effective intent-to-donate were similar in both groups (94.8% females vs. 94.6% males). At enactment, a lower proportion of people 65+ had registered an opt-in decision (40.3%) relative to other age groups (19-29 = 54.6%; 30-48 = 59.8%; 49-64 = 54.4%). One year following enactment, rates of effective intent-to-donate were similar in all age groups (19-29 = 94.7%; 30-48 = 95.7%; 49-64 = 94.6%; 65+ = 92.5%).
Conclusion: This work evaluates the impact of deemed consent legislation on effective intent-to-donate in Nova Scotia. Enactment of deemed consent legislation increased rates of effective intent-to-donate and appears to have mitigated pre-existing differences by gender and age group. Future research into the relationship between the dramatic increase in rates of effective intent-to-donate and consent rates is ongoing.
References:
1) Steffel, M., Williams, E. F., & Tannenbaum, D. (2019). Does changing defaults save lives? Effects of presumed consent organ donation policies. Behavioral Science & Policy, 5(1), 68-88.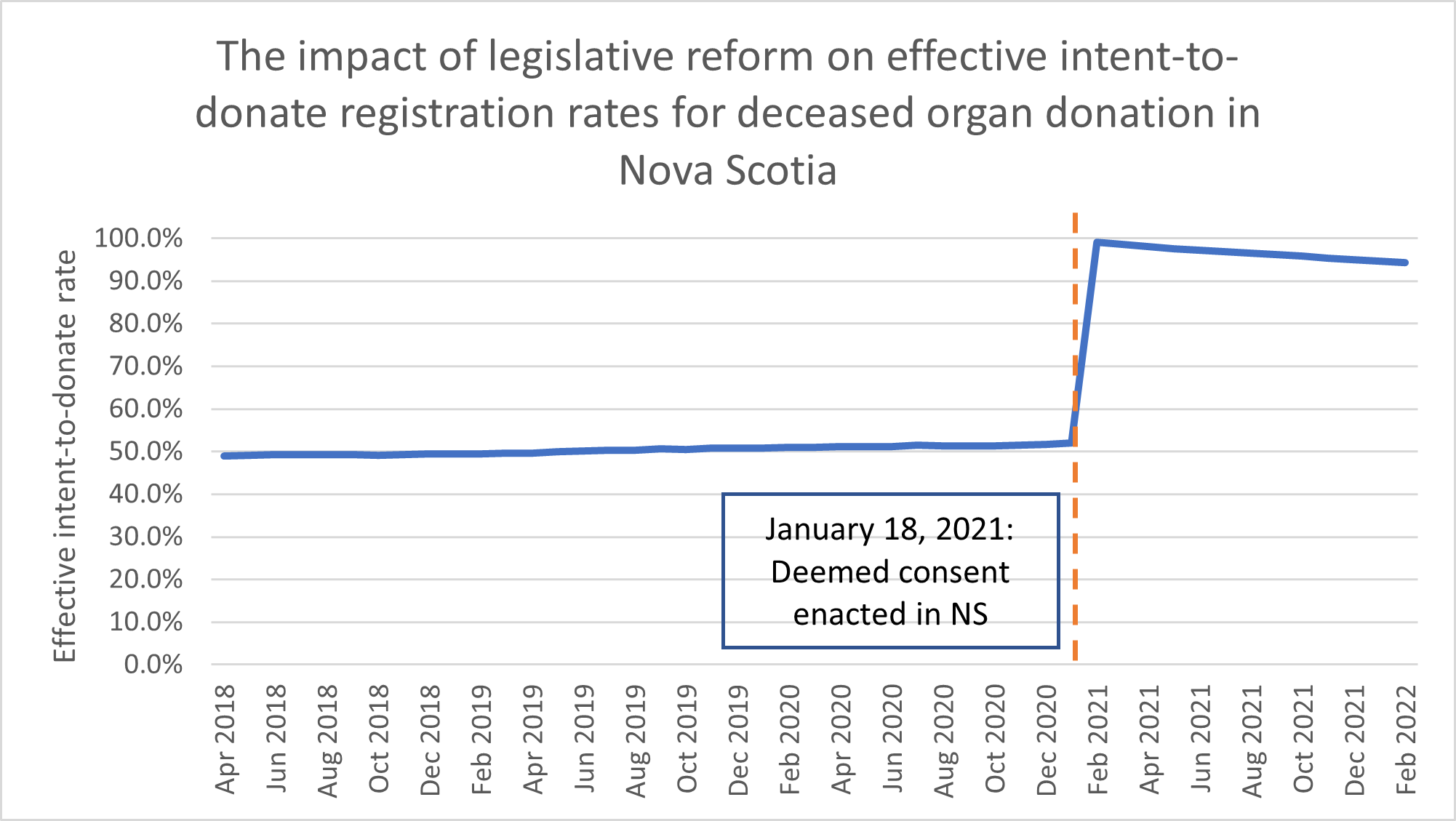
Health Canada, Health Care Policy Contribution Grant through the Organ Donation and Transplantation Collaborative.

right-click to download
