One organ procurement organization's effective strategy for dramatically increasing donation after circulator death donation and transplantation
Jacqueline Giuffrida1, Gweneth O'Shaughnessy BA1, Elizabeth Brown RN, BSN, CPTC2, John Edwards RN, BSN, RRT, CPTC2, Christine Radolovic MS, BSN, CPTC1,2, Richard Hasz MFS, CPTC1,2.
1Hospital Development, Gift of Life Donor Program, Philadelphia, PA, United States; 2Transplant Coordinator Services, Gift of Life Donor Program, Philadelphia, PA, United States
Introduction: Donation after circulatory death (DCD) represents a viable organ donation option in scenarios where a patient doesn’t meet strict brain death criteria. DCD has been proven to increase the supply of donor organs for transplantation. DCD has been a standard of practice for over two decades in this Organ Procurement Organization, ensuring that every opportunity to honor a patient’s decision or to offer donation to a family was fully explored.
Methods: In 2021, the United Network for Organ Sharing (UNOS) led a ‘DCD Collaborative’. This OPO was one of 36 participants. The goal was to increase DCD 20%. To achieve the goal this OPO created and implemented an improvement strategy: 1. Establishing OPO metrics and key performance indicators; 2. Implementing an Improvement Team (seven Transplant Surgeons, seven Critical Care Physicians) responsible for driving results; 3. Formation of distinct ‘work groups’ to implement specific tactics (DCD physician survey, DCD resource guide, normothermic regional perfusion model, uncontrolled DCD hospital protocol); 4. Internal OPO strategy and collaboration within Transplant Coordinator and Hospital Development departments.
Results: Engagement was maintained through ‘DCD Improvement Team Meetings’ where a standardized agenda was utilized. Daily surveillance by Administrators on Call (AOC) guided clinical practice to rule-in every possible potential DCD candidate. A retrospective quality process was implemented to review rationale for ruling out patients as DCD candidates. Sharing of this information occurred at weekly AOC meetings. Customized data analytics were used to monitor outcomes and progress.
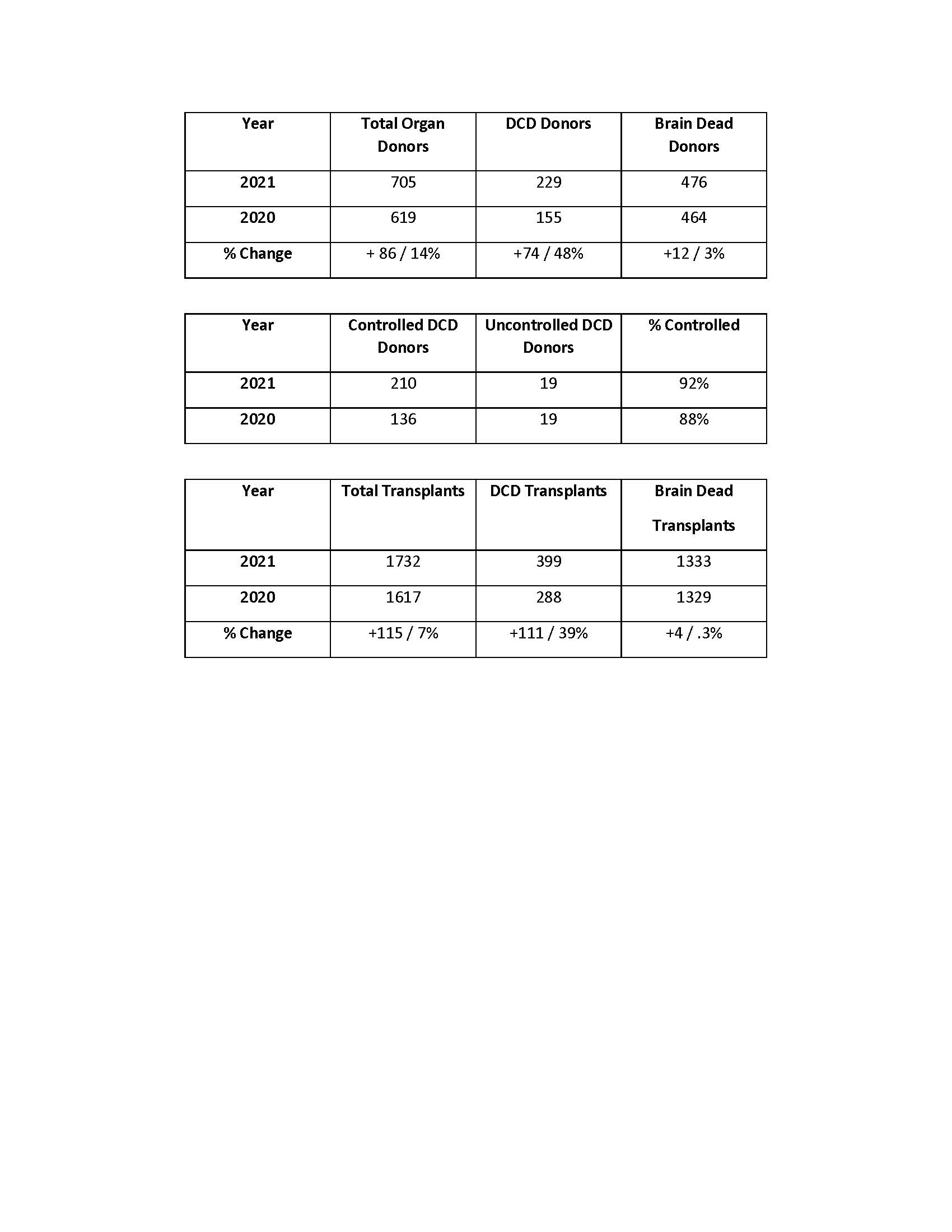
This OPO achieved a 48% increase in DCD donation and a 39% increase in DCD transplants. As a result of Hospital Development messaging for clinical referral triggers and aggressive clinical practice, the pool of potential DCD donors increased by 43%. Additionally, the focused education on preserving the donation opportunity resulted in an increase in the percentage of DCD cases that were facilitated in a controlled fashion. The OPO surpassed its goal of coordinating 30 DCD liver transplants. Authorization rates for DCD improved from 47% in 2020 to 51% in 2021. Twelve Improvement Team meetings and two physician-led DCD webinars occurred. Normothermic regional perfusion model protocol was adopted. A DCD physician survey was completed. Feedback is being incorporated into a DCD Resource Guide developed by the critical care physician work group.
Conclusion: Establishing clear goals, a comprehensive strategy and tactics created an environment that fostered focused attention on every referral of a potential DCD candidate. Incorporating active and retrospective quality components allowed OPO staff to be agile, adjusting clinical decisions quickly. Communication across OPO departments promoted idea sharing leading to robust team meetings and educational programming. Processes established during this initiative have been adopted as standards of practices.

right-click to download
