
Hematopoietic cell transplantation from volunteer unrelated donor between 2016 and 2021: a collaborative study GATMO-TC and INCUCAI
Ana Basquiera1, Richard Malan2, Raquel Staciuk1, Mariano Berro1, Vera Milovic1, German Stemmelin1, Monica Makiya1, Mariel A Perez1, Leandro Riera1, Martin Saslavsky1, Javier Bordone1, Maria C Foncuberta1, Georgina Bendek1, Sandra Formisano1, Nicolas Fernandez Escobar1, Jorge A Alberbide1, Jorge H Milone1, Gregorio Jaimovich1, Diego Larriera2, Carlos A Soratti2, Pablo Galarza2.
1Grupo Argentino de Trasplante de Médula Ósea y Terapia Celular (GATMO-TC), Sociedad Argentina de Hematología, Buenos Aires, Argentina; 2Registro Nacional de Donantes de Células Progenitoras Hematopoyéticas (CPH), Instituto Nacional Central Único Coordinador de Ablación (INCUCAI), Buenos Aires, Argentina
Introduction: Hematopoietic cell transplantation (HCT) from HLA-matched (MUD) or HLA-mismatched unrelated donors (MMUD) offers a curative strategy for patients with many malignant and benign hematological diseases. However, the success of HCT may be limited because of graft versus host disease, graft failure, and relapse disease. We aimed to describe donor´s and recipient´s features, and their association with survival, for patients who underwent a MUD and MMUD in Argentina between 2016 and 2021.
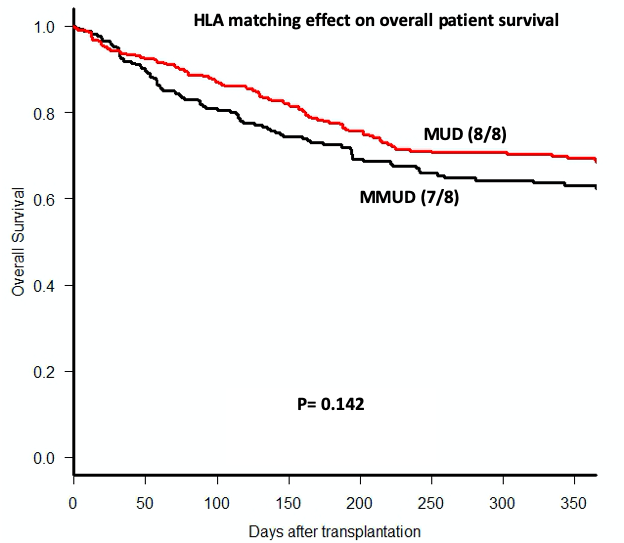
Methods: We used data from a national database (SINTRA) for HCT managed by Instituto Nacional Central Único Coordinador de Ablación (INCUCAI). These data were confronted by another database from unrelated donors also from INCUCAI. All transplant centers are affiliated to Grupo Argentino de Trasplante de Médula Ósea y Terapia Celular (GATMO-TC). Only a first HCT with a volunteer unrelated donor was included, both MUD and MMUD using high-resolution HLA. Patients who underwent transplants with umbilical cord blood (UCB) were excluded. Overall survival (OS) was estimated by Kaplan-Meier curves and compared by log-rank test.
Results: A total of 617 cases (median age 18 years; range 0.5-73; 287 cases less than 16 years old) were included: 2016 n=80, 2017 n=97, 2018 n=116, 2019 n=134, 2020 n=84, y 2021 n=106. Main diagnostics were: acute lymphoblastic leukemia (ALL) n=161, acute myeloblastic leukemia (AML) n=125, myelodysplastic syndrome (MDS) n=88, immunodeficiencies n=74, aplastic anemia n=53, myeloproliferative neoplasms (MPN) n=29, and non-Hodgkin lymphoma n=19. In the group of patients less than 16 years old, the more frequent diagnosis was ALL (33%) followed by immunodeficiencies (24%); in patients older than 16 years old, AML (27%) and MDS/MPN (25%). Stem cell source was peripheral blood in 473 cases (77%). Considering four HLA-locus studied, donors were 6/8 n=4, 7/8 n=254, and 8/8 n=357, By considering also DQB1, the donors were 8/10 n=12, 9/10 n=259 (13 with DQB1 mismatched), and 10/10 n=344. Donors (median age 30 years) were from: Germany n=224, Argentina n=140, EEUU n=90, Brazil n=42, Poland n=25, Israel n=18, Spain n=14, Great Britain n=11, Chile n=9, Italy n=9, Switzerland n=7, Turkey n=7, Portugal n=6, France n=4, The Netherlands n=3, Austria n=1, Canada n=1, China n=1, Sweden n=1, Thailand n=1. The proportion of Argentinian donors was increasing along the calendar year since 10% in 2016 to 28% in 2021. Median of follow-up for the surviving cohort was 365 days (IQR 176-730). One-year OS was 66% (95%CI 62-70). No difference was found in terms of OS regarding age and sex recipient, donor/recipient sex matching, benign and malignant diseases, stem cell source, and between MMUD and MUD (Fig1).
Conclusions: HCT with a volunteer unrelated donor is a feasible treatment in our country, even considering mismatched donors. A third of donors were coming from Argentina highlighting the role of the national donor’s registry in our country.

right-click to download
