Outcomes of single kidney transplantation from pediatric donors with acute kidney injury into pediatric recipients
Qiang Zhang1, Jun Li1, Mingchuan Huang1, Wenrui Wu1, Chenglin Wu1, Qian Fu1, Huanxi Zhang1, Xiaojun Su1, Longshan Liu1, Changxi Wang1,2.
1Department of Organ Transplant, The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, People's Republic of China; 2Organ Donation and Transplant Immunology, Guangdong Provincial Key Laboratory, Guangzhou, People's Republic of China
Background: Despite the potential reversibility of acute kidney injury (AKI) lesions, kidneys from AKI pediatric donors are underutilized especially for pediatric recipients. Single kidney transplantation from small pediatric donors to pediatric recipients (PTP) can maximize the number of recipients. The objective of this study is to test whether pediatric recipients transplanted with single AKI pediatric kidneys achieve comparable results to other PTP patients.
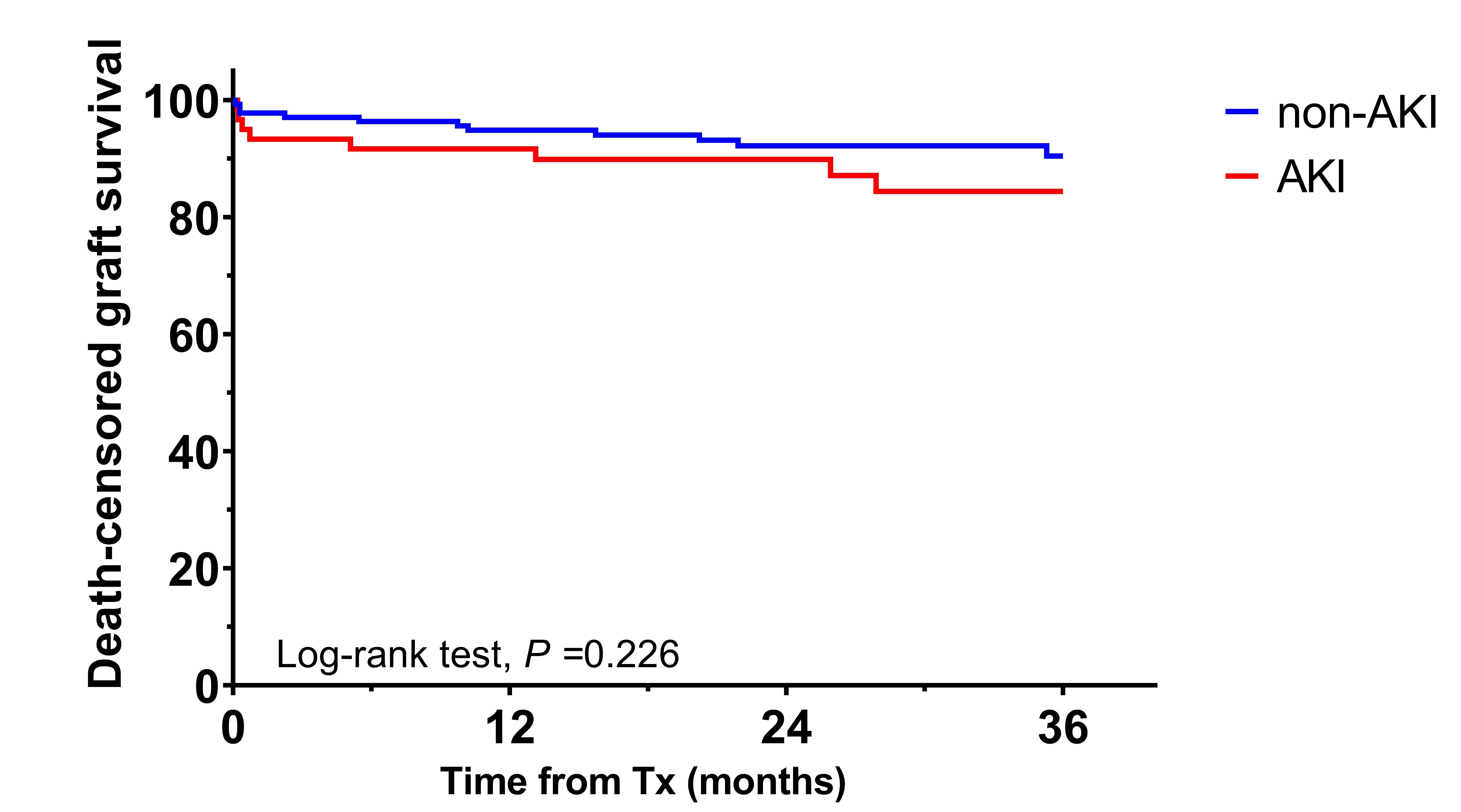
Methods: This retrospective cohort study investigated all single kidney transplantation PTP patients between 01/2012 and 12/2020 in a single specialized transplant center. AKI was defined by the pediatric-modified RIFLE criteria. Outcomes were compared using Kaplan-Meier with log-rank test and death-censored graft survival was assessed by multivariable Cox proportional hazard model. The study was approved by the ethics committee of The First Affiliated Hospital, Sun Yat-sen University.
Results: Of all 197 enrolled patients, 60 (30.46%) were transplanted from AKI donors and 137 (69.54%) from non-AKI donors. Patients were followed for a median of 31 months (range, 12-108 months) after transplantation, during which 24 (12.18%) grafts were lost, and 2 (1.02%) patients died of pulmonary infection. Rejection (50%) was the leading cause of graft loss followed by vascular thrombosis (20.83%) and recurrent disease (12.5%). No significant difference was found between the two groups on the incidence of acute rejection over time (P = 0.1597). Primary nonfunction was observed only in one patient from the AKI group. Delayed graft function occurred equally between two groups (16.67% vs. 13.87%, P = 0.61). All groups demonstrated satisfactory graft function, eGFR at 3 years post-transplant was 84.6±22.63, 91.03±33.25mL/min/1.73m2 for AKI and non-AKI groups, respectively (P = 0.441). Three-year death-censored graft survival in the AKI group was 83.33%, comparable to the results in the non-AKI group (89.78%, P = 0.226). The adjusted hazard ratio (aHR) for graft loss was similar for recipients of AKI (aHR 1.48, 95% CI 0.65-3.35, P = 0.348) compared with the non-AKI group.
Conclusions: Single kidneys from AKI pediatric donors have at least as good outcomes as non-AKI pediatric donors when transplanted into children. This study provides evidence to support the use of AKI pediatric donors for pediatric single kidney transplantation.
Reference:
1. Xu, X., et al., Acute Kidney Injury among Hospitalized Children in China. Clin J Am Soc Nephrol, 2018. 13(12): p. 1791-1800.
2. Pereira, L. and P.C.K. Nogueira, Non-standard Criteria Donors in Pediatric Kidney Transplantation. Pediatr Transplant, 2019. 23(5): p. e13452.
3. Jiang, Z., et al., Pediatric Donor Glomerulopathy Is a Possible Cause of Abnormal Urinalysis in Adults Receiving Small Pediatric Donor Kidneys. Transplantation, 2020. 104(8): p. 1695-1702.
4. Troppmann, C., et al., Short- and Long-term Outcomes of Kidney Transplants From Very Small (</=15 kg) Pediatric Donors With Acute Kidney Injury. Transplantation, 2021. 105(2): p. 430-435.

right-click to download
