The impact of COVID-19 on pediatric organ donation and transplantation
Thomas Nakagawa1, Eliza J Lee2, Xingyu Zhang3, George Mazariegos2.
1Pediatrics, Division of Pediatric Critical Care Medicine, University of Florida College of Medicine-Jacksonville, Jacksonville, FL, United States; 2Department of Surgery, Division of Transplant Surgery, University of Pittsburgh Medical Center, Pittsburgh, PA, United States; 3Thomas E. Starzl Transplantation Institute, University of Pittsburgh Medical Center, Pittsburgh, PA, United States
Purpose: The global COVID-19 pandemic has significantly altered delivery of healthcare. Hospital resource utilization has been impacted on multiple levels including solid organ transplantation and overall access to transplant care. In the United States, significant regional variation and decreased living donor transplantation occurred during the initial 6 months of the pandemic. We examined the multi-year impact of COVID-19 on pediatric organ donation and transplantation.
Methods: Pediatric (<18 years of age) organ donation and transplant data was obtained from the Organ Procurement and Transplantation Network (OPTN). Data were reviewed between January 2019 to December 2021 and included pediatric donors after brain death (pDBD), donors after circulatory death (pDCD), living donors (LD), and recipient details including total number of transplants, waitlist deaths, and removals.
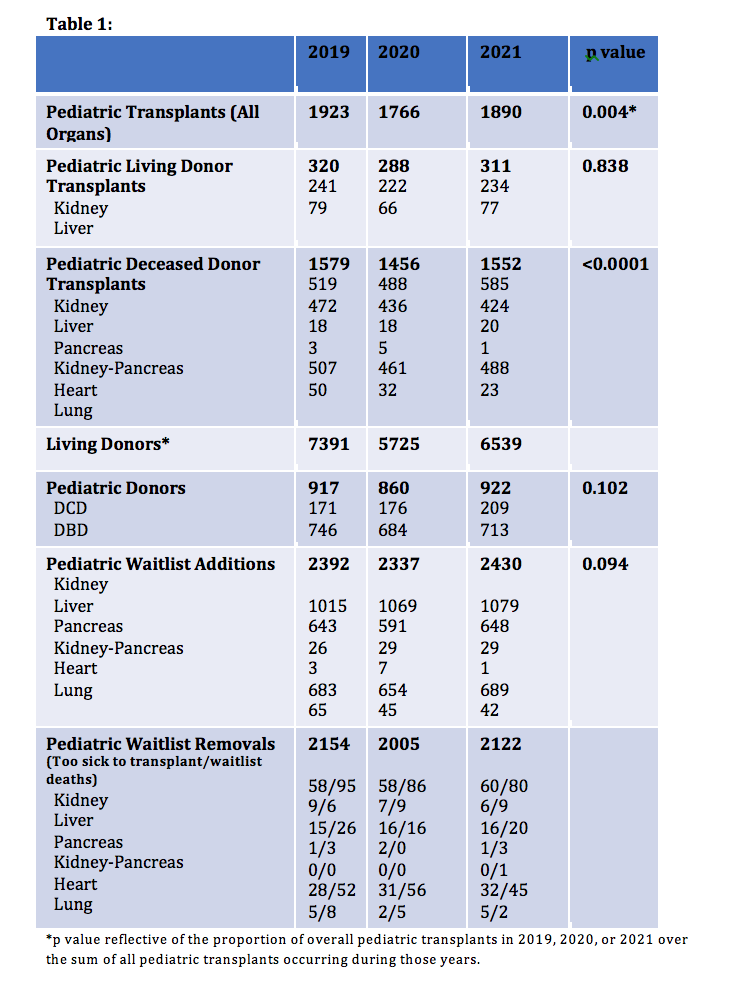
Results:Total pediatric transplants performed in 2019, 2020, and 2021 were 1923, 1766, and 1890 (p=0.004) respectively. Organ specific data is outlined in Table 1. In 2019, 2020, and 2021, living donor transplantation accounted for 320, 288, and 311 (p=0.838) cases, while 1579, 1456, and 1552 (p=<0.0001) deceased donor allografts were utilized. There were 171, 176, and 209 pDCD and 746, 684, and 713 pediatric pDBD donors. Living donors across all recipient ages were 7391, 5725, and 6539. Pediatric patients added to all organ waitlists during the study period were 2392, 2337, and 2430. Children removed from the waitlist for all conditions were 2347, 2198, and 2288 with 93, 82, and 76 of those cases due to patient death. There was no statistically significant difference in the proportion of pediatric patients added to the waitlist compared to those removed during 2019-2021 (p=0.505).
Conclusions: Transplant volume transiently decreased in the first six months of the COVID-19 pandemic. However, transplantation rates in children, specifically abdominal organ transplantation, increased to nearly pre-pandemic levels in 2021. Lung transplants were significantly decreased during the study period. Pediatric donation remained relatively steady from 2019-2021. Living donor transplantation in children was significantly impacted in 2020. Waitlist additions/removals remained consistent throughout the study period.

right-click to download
