Results of 922 pediatric liver transplants: prognostic factors, learning curve and impact on one-year survival
Maria Julia Minetto1, Guillermo Cervio1, Marcelo Dip1, Esteban Halac1, Leandro Lauferman1, Diego Aredes1, Agustina Jacobo Dillon1, Hayellen Reijenstein1, Florencia D´Arielli1, Miguel Palmeiro1, Javier Goñi1, Oscar Imventarza1.
1Liver Transplantation, Garrahan Hospital, Buenos Aires, Argentina
Objective: The objective of this work is to analyze the impact on one-year survival of pediatric liver transplanted patients during 29 years of the transplantation program at the “Prof. Dr. J.P. Garrahan ”.
Materials and Methods: 922 pediatric liver transplants were retrospectively studied, including prognostic factors and the experience curve, and comparing two different stages: Era I (1992-2005) and Era II (2005-2021). Pre, intra and post-transplant variables were defined. A univariate and multivariate logistic regression analysis was performed to evaluate the predictors of mortality and graft loss at one year.
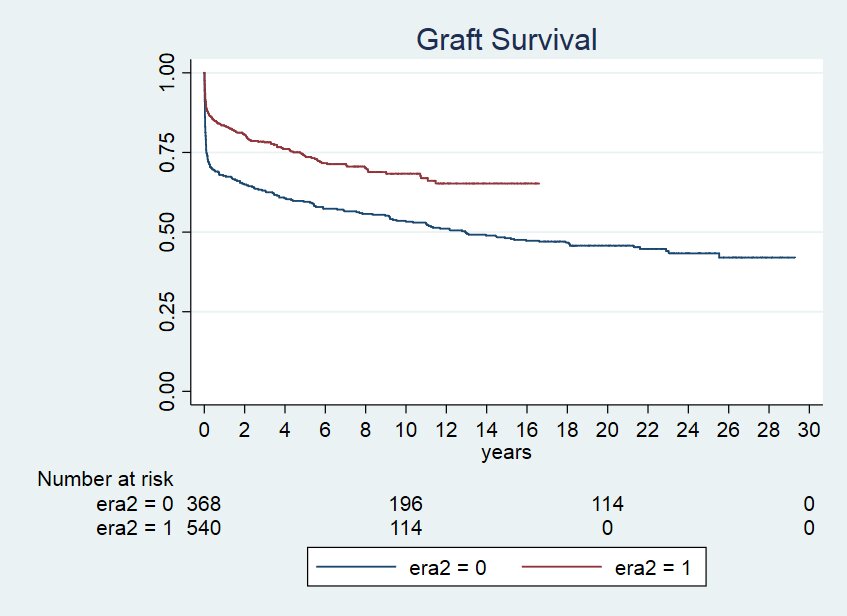
Results: The median weight of patients was 13 kg and the most frequent indication for transplantation was biliary atresia (35%). The living related donor represented 27% of the transplants and those performed with cadaveric liver were: with whole liver (34%), reduced (24%) and split (16%). The overall survival of the patient and the graft at one year was 79.75% and 75.54%, respectively. The risk factors for patient death and graft loss one year after transplantation in the multivariate analysis were: child under 10 kg at the time of transplantation, late retransplantation, liver reduction technique, use of an arterial graft, primary non function and arterial thrombosis. In Era I, there was a greater number of transplants in emergency status, a longer cold ischemia time, a lower number of late retransplants, and a lower delayed closure of the abdominal wall. Overall graft and patient survival at one year improved significantly in Era II from 66.94% to 81.56% (log rank 0.0000) and from 70.88% to 86.30% (log Rank 0.0000), respectively.
Conclusion: The present work demonstrates the evolution in the learning curve over a 29 year period and its relationship with the improvement on early post-transplant survival in a transplant program that takes place in a public hospital in Argentina. The improvements achieved during the second ERA of the program are comparable to international standards and reflect the continuous improvement and experience of an interdisciplinary team." href="https://cm.tts2022.org/papers/body/1508#">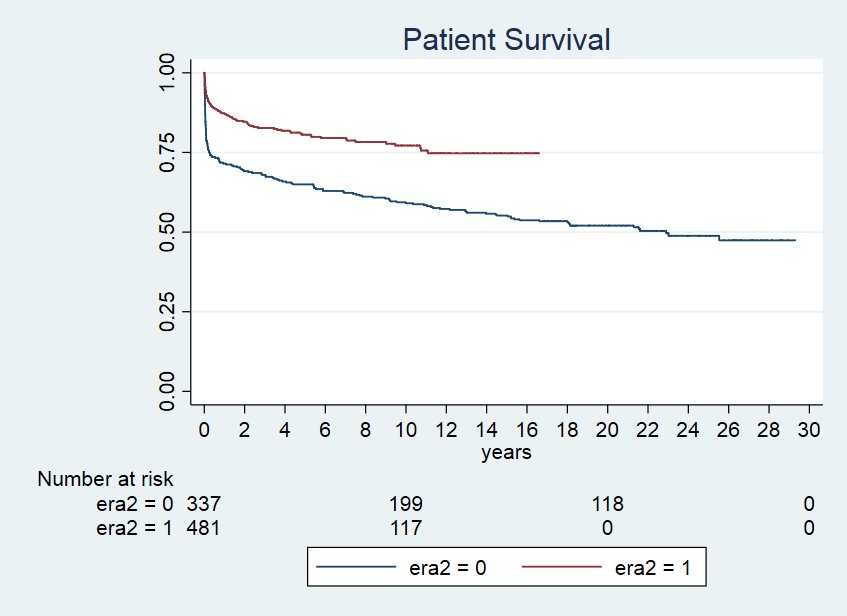

right-click to download
