A pre-transplant risk assessment tool for outcome in pediatric kidney transplantation based on a Dutch cohort of 1415 patients
Loes Oomen1, Huib de Jong2, Antonia HM Bouts3, Mandy G Keijzer-Veen4, Elisabeth AM Cornelissen5, Liesbeth L de Wall1, Wout FJ Feitz1, Charlotte MHHT Bootsma-Robroeks5,6.
1Pediatric Urology, Radboudumc Center Amalia Children's Hospital, Nijmegen, Netherlands; 2Pediatric Nephrology, Erasmus MC-University Medical Centre, Rotterdam, Netherlands; 3Pediatric Nephrology, Amsterdam University Medical Center, Emma Children's Hospital, Amsterdam, Netherlands; 4Pediatric Nephrology, Wilhelmina Children's Hospital, University Medical Center Utrecht, Utrecht, Netherlands; 5Pediatric Nephrology, Radboudumc Center Amalia Children's Hospital, Nijmegen, Netherlands; 6Pediatric Nephrology, UMC Groningen Beatrix Children’s Hospital, Groningen, Netherlands
Background: Donor allocation is an important modifiable factor in pediatric kidney transplantation. A prediction model based on donor characteristics could help optimize graft survival. The aim of this study is to develop a risk assessment tool for graft loss based on essential pre-transplantation characteristics.
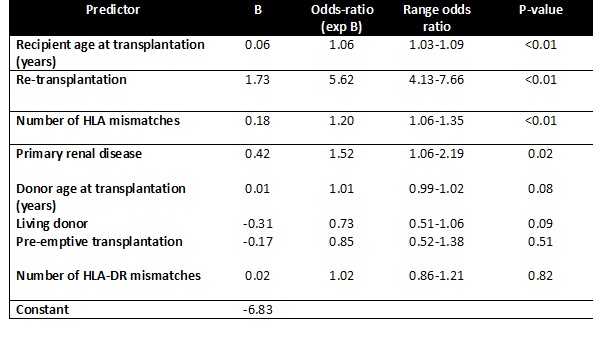
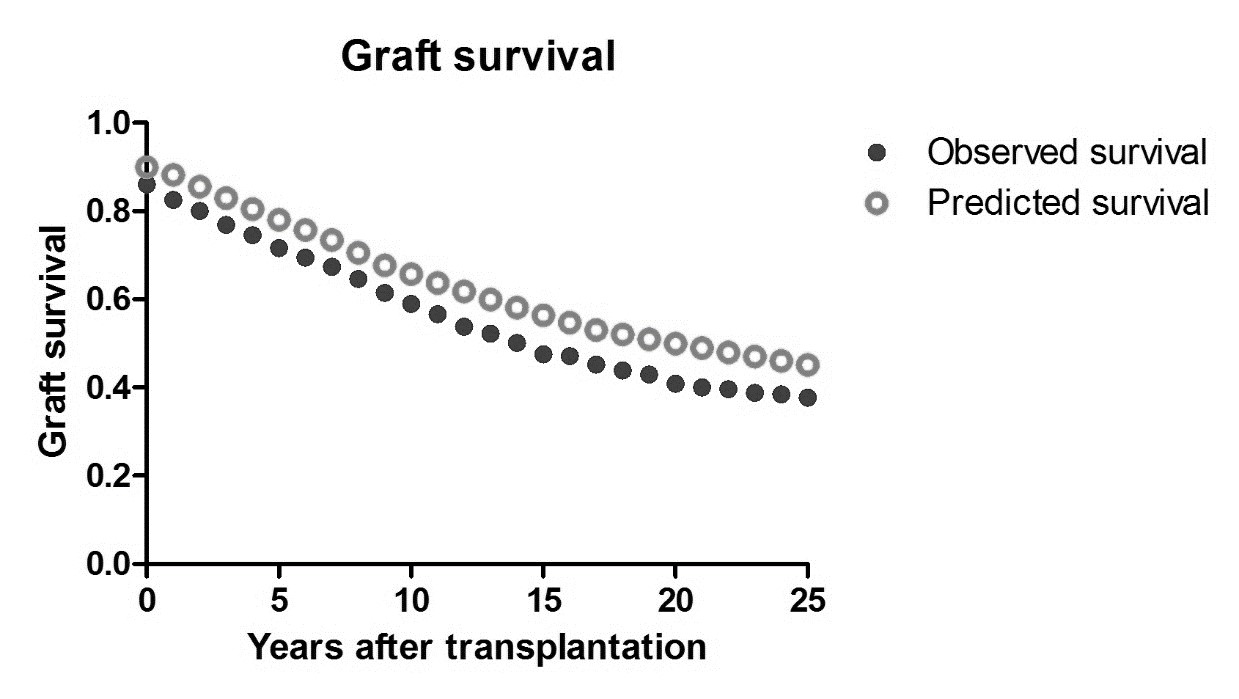
Methods: A prospective Dutch registry was used including all transplantation data since 1966. A multivariable binary logistic model with discrete-time event history analysis was used to predict hazard of graft loss. This model was corrected for era of transplantation and course of time after transplantation. Subsequently, a prediction score was calculated based on the B-coefficients. For internal validation a derivation (80%) and validation cohort (20%) were defined. Performance of the model was assessed with area under the curve (AUC) of the receiver operating characteristics curve (ROC), Hosmer-Lemeshow test and calibration plots.
Results: The prediction model was based on 7252 observations after 1415 transplantations in patients [age 1-18] between 1966-2021. 10-years graft survival was 42% for transplantations before 1990 and improved to a current 92%. Over time significantly more living and pre-emptive transplantations and increased donor age were seen (p<0.05). Other variables included in the model were recipient age, number of previous transplantations, number of HLA mismatches, era of transplantation and underlying renal disease. The predictive capacity of this model was very good with AUC scores of 0.81, 0.78, 0.77 and 0.74 after 1, 5, 10 and 20 years respectively (p<0.01). Calibration plots showed excellent fit.
Conclusion: This pediatric pre-transplant risk assessment tool was shown to be highly predictive for graft survival in the Netherlands. This model uses essential variables and could support decision making regarding donor selection and optimizing graft outcome.

right-click to download
