Total bilateral arm transplantation: functional recovery and psychosocial outcomes at one year
Palmina Petruzzo2, Laure Huchon1, Christian Seulin5, Eleonore Daux5, Aram Gazarian4, Marion Charvin1, Gilles Rode1, Jean Kanitakis3, Patrick Feugier6, Lionel Badet2, Emmanuel Morelon5.
1Service de médecine physique et réadaptation, Hospices Civils de Lyon, Saint Genis Laval, France; 2Department of Transplantation Surgery, Hopital Edouard Herriot, Hospices Civils de Lyon, Lyon, France; 3Department of Dermatology, Hopital Edouard Herriot, Hospices Civils de Lyon, Lyon, France; 4Service de chirurgie orthopédique du membre supérieur,, Hopital Edouard Herriot, Hospices Civils de Lyon, Lyon, France; 5Transplantation, nephrology and clinical immunology, Hopital Edouard Herriot, Hospices Civils de Lyon, Lyon, France; 6Vascular surgery, CHLS, Hospices Civils de Lyon, Pierre Benite, France
Introduction: Although arm loss causes severe disability and compromission of body image, functional recovery after allotransplantation still presents many challenges.
Objective: A bilateral arm transplantation including reconstruction of the left shoulder was performed on January 13, 2021 in Lyon (France). Functional recovery and psychosocial outcomes are reported one year after the transplantation.
Materials and Methods: The recipient was a 48-year old patient with bilateral amputation at proximal arm level after electric shock in January 1998, who underwent liver transplantation in 2002. The patient used mechanic prostheses with poor satisfaction. The surgical procedure consisted in a total arm transplantation on the left side with reconstruction of the gleno-humeral joint. The maintenance immunosuppressive therapy included tacrolimus, mycophenolate mofetil and prednisone. Rehabilitation therapy started on day one. It progressively included manual lymphatic drainage, passive motion of all joints in a total range except limitations for the shoulders during the first 6 weeks. Then, electrostimulation on denervated muscles was performed. After 6 weeks the protocol included hand therapy, psychomotricity, physical activities, occupational therapy and sensory-motor simulation training approaches (motor imagery, virtual mirror therapy, virtual reality).
Results: Motor recovery was already appreciated 8 months after the transplantation. At one year, passive ranges of motion of upper limbs are subnormal. According to MRC scale, muscular strength at shoulder level is from 3 to 4/5 on the right side and from 1 to 2/5 on the left side; from 3 to 4/5 for elbow flexors and from 1 to 2 for elbow extensors on both sides; 3/5 for wrist flexors on the right side and 0/5 on the left side; 1 to 2/5 for wrist extensors on both sides; 3/5 for pronators and supinators on the right side and 1/5 on the left side. Slight contraction and movements of the extrinsic flexors and extensor muscles of the fingers have been evidenced on both sides, and the first prehension movements started on the right hand.
The Semmes-Weinstein monofilament test for sensory threshold was 6.65 in the right palm and below the left elbow; deep pressure sensation is recovered in both hands. Functional Independence Measure is 96/126 and the DASH score 75.8. The patient is able to perform the same daily activities as with the prostheses before the transplantation.
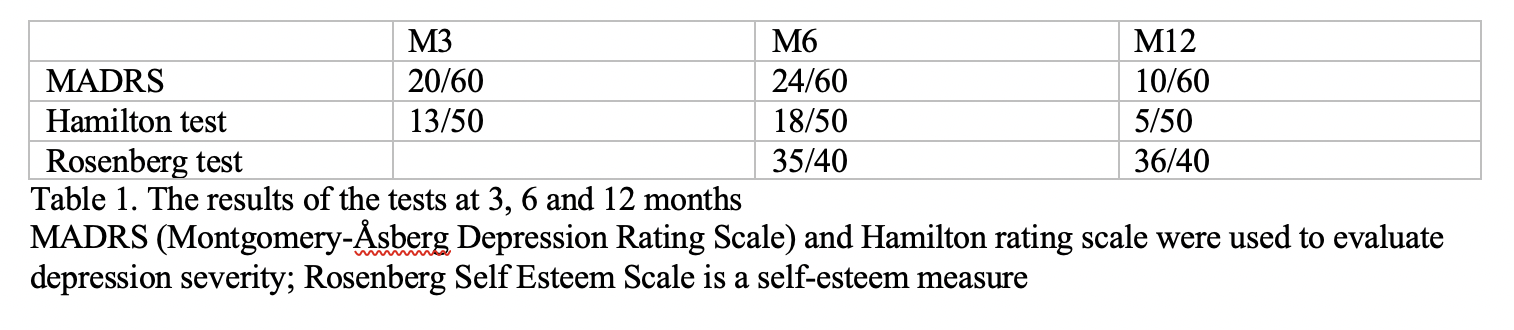
The patient was psychologically tested during the follow-up using a specific questionnaire for upper extremity allotransplantation and MADRS, Hamilton and Rosenberg tests. The results (Table 1) show the difficulties, the patient’s strong motivation and capacity to cope, and his satisfaction reached at the first year of follow-up.
Conclusions: The patient is very satisfied of his grafts and of his restored body image, which was his main expectation.

right-click to download
