
Long term results on intestinal rehabilitation of children treated at a single multidisciplinary unit
Carolina Rumbo1, Maria I Martinez1, Julio Trentadue2, Dolores Garcia2, Gabriel E Gondolesi1.
1Intestinal Transplant, Hospital Universitario Fundacio Favaloro, Buenos Aires, Argentina; 2Pediatrics, Hospital Universitario Fundacio Favaloro, Buenos Aires, Argentina
Background and aim: IF is a chronic condition with high morbidity. Intestinal rehabilitation can be enhanced when patients are treated by specialized multidisciplinary teams. We aim to show the long-term results of a group of children with SBS and chronic IF treated with a comprehensive approach at a single IF and transplant unit.
Material and methods: Retrospective review of a prospectively filled database of pediatric patients with chronic IF secondary to SBS (≤ 40 cm of remnant small intestinal length- RSIL) seen from May 2006 to December 2021. Patients were grouped according to the intestinal rehabilitation outcome; for survival analyses, late referrals were excluded. Data was analyzed using SPSS,v20.0.
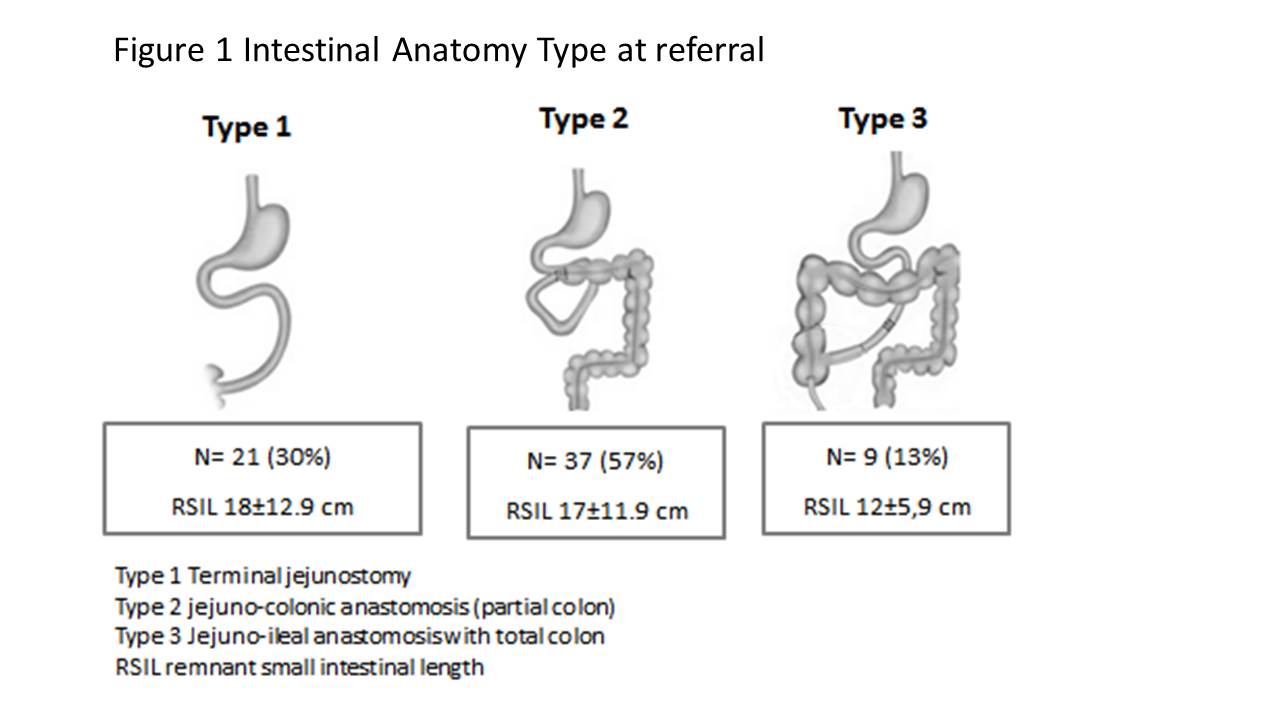
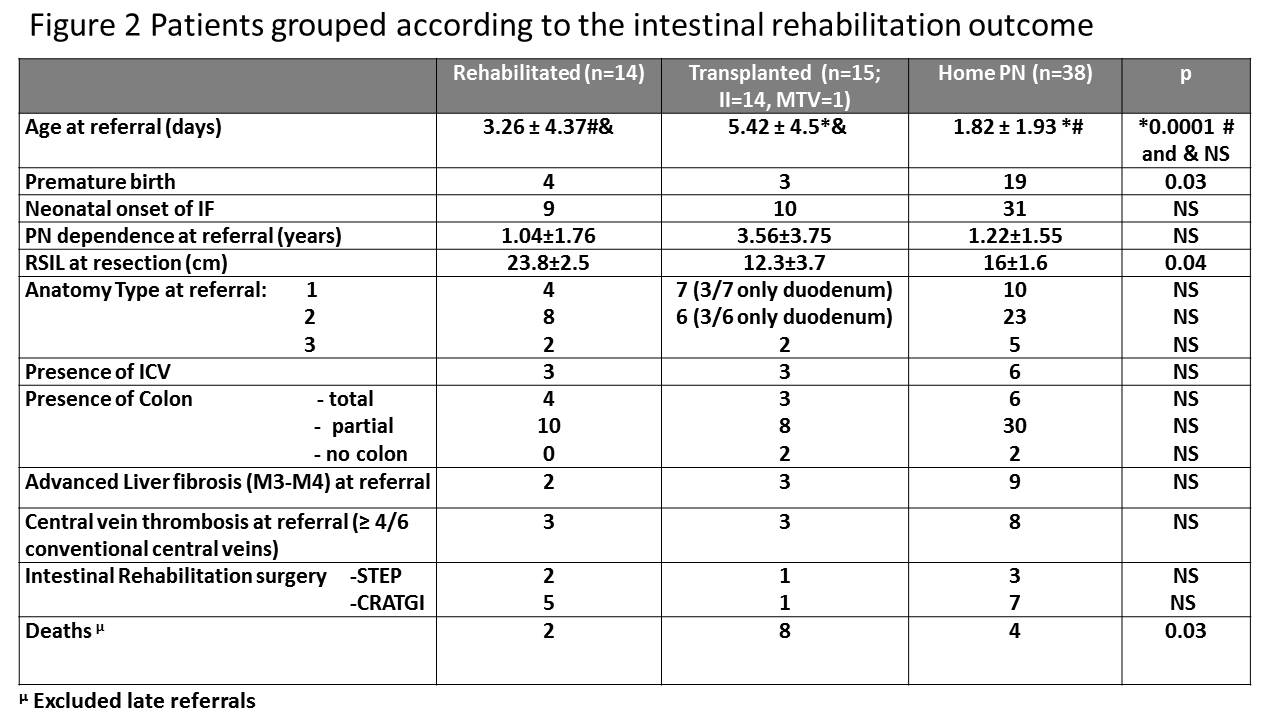
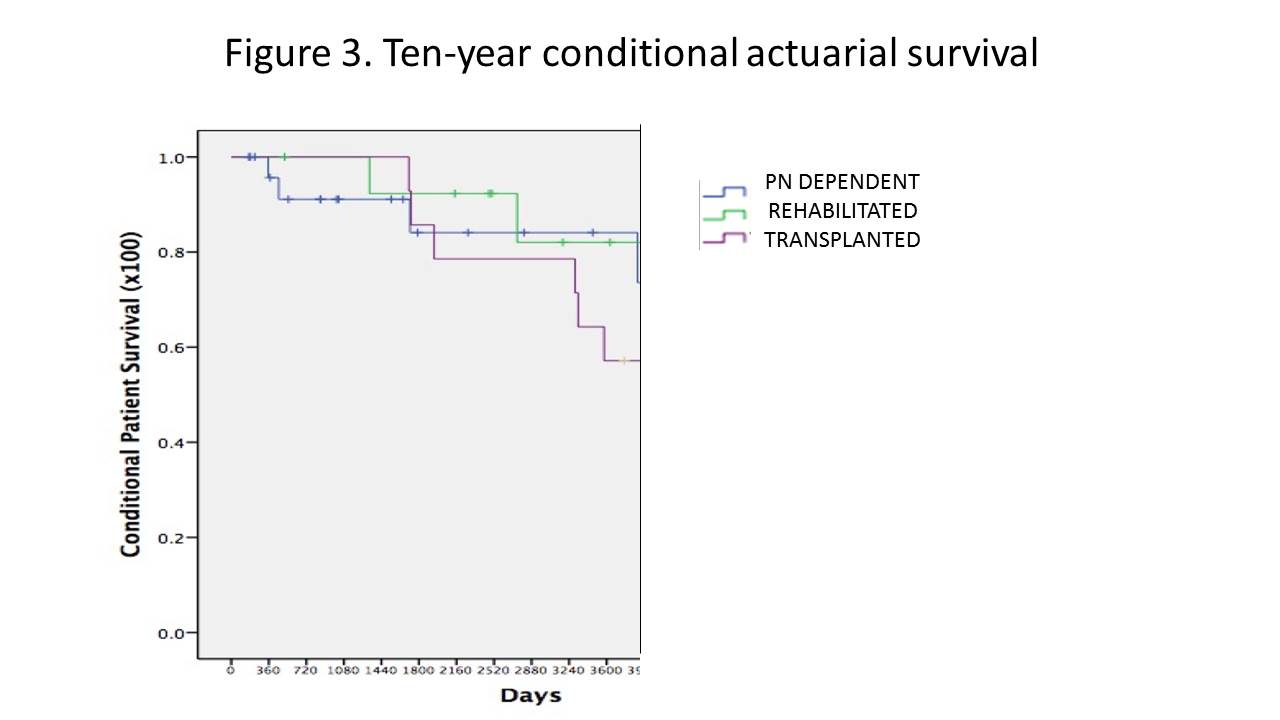
Results: 67 patients were included; 46 (69%) male, 25 (37%) premature (mean gestational age 33.5 weeks), 55 (82%) had neonatal onset of IF. Etiologies were: gastroschisis (31%), intestinal atresia (22%), volvulus (19%), long segment Hirschsprung's disease (7.5%), NEC (6.5%); post-surgical complications (5%) and others (9%). Median RSIL at the time of resection was 16.7±11.7 cm; intestinal anatomy type is shown in figure 1. Mean age at first consult was 2.93±3.51 years. At referral, mean time of PN dependency was 623±890 days, mean PN support 113% of the estimated basal metabolic rate for age. Fourteen (21%) had extensive central venous thrombosis and 16 (24%) had advanced fibrosis on liver biopsy. At the cut off day of analysis, 14 (21%) achieved intestinal rehabilitation, and 9 (13%) had at least 20% reduction of PN support. Twelve (32%) of those that remained PN dependent were included on the waiting list at referral and died shortly after thus are considered late referral. Fifteen (22.5%) underwent Intestinal transplantation (ITX) 14 Isolated, 1 MTV (figure 2). Ten-year conditional actuarial survival of the series was 72% (figure 3)(84% for PN dependent, 82% for rehabilitated patients and 57% for ITX recipients).
Conclusions: IR is possible even in very short gut or unfavorable anatomy when care is provided by a multidisciplinary team. Timely referral to specialized units results in diverse alternatives to reduce PN support and increases survival.

right-click to download
