Closing the gap: addressing inequities in access to kidney transplantation for Aboriginal Australians from the Kimberley region
Anoushka Krishnan1, Doris Chan2, Wai H. Lim2, Calina Ting2, Tarryn Isard2, Nicholas Corsair3, Emma Griffiths4, James Stacey4, Rebecca Bartlett1, Kelli Owen5, Denise Fallon1, Bryon Jaques2, Khalil Patankar1.
1Nephrology, Royal Perth Hospital, Perth, Australia; 2Nephrology, Sir Charles Gairdner Hospital, Perth, Australia; 3Kimberley Renal Services, (KRS), Broome, Australia; 4Kimberley Aboriginal Medical Services, (KAMS), Broome, Australia; 5National Community Engagement Coordinator, South Australian Health and Medical Research Institute, Adelaide, Australia
Introduction: Aboriginal and Torres Strait Islander people are at higher risk of developing chronic kidney disease, particularly those in remote areas, when compared with non-Indigenous Australians. While the number of Indigenous Australians requiring kidney replacement therapy has increased over time, rates of kidney transplantation (KTx) in prevalent patients has remained low at 14% compared with 50% in non-indigenous Australians.
Methods: The National Indigenous Kidney Transplant Taskforce (NIKTT) was established in 2018 in response to the disproportionately low rates of KTx among Aboriginal and Torres Strait Islander people in Australia. We describe the outcomes of a NIKTT-sponsored initiative developed by the teams at Sir Charles Gairdner Hospital, Royal Perth Hospital and Kimberley Aboriginal Medical Service aimed at identifying and addressing modifiable barriers to accessing KTx for Aboriginal Australians with kidney failure in the Kimberley, Western Australia. This remote area which is over 1000 km from the capital city of Perth and spans a vast area of northwest Western Australia caters to the dialysis needs of over 150 Aboriginal Australians.
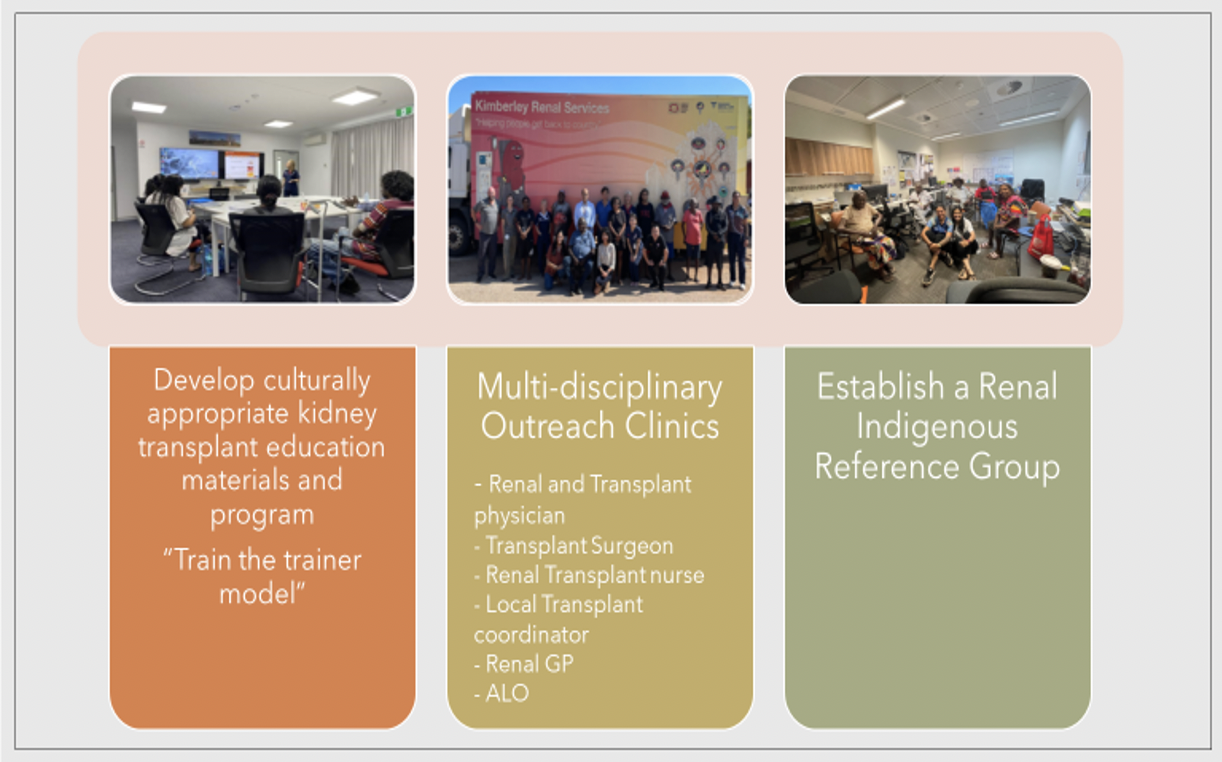
Results: A multi-pronged approach was used. Culturally appropriate KTx education modules were developed for patients and health professionals in close consultation with Aboriginal liaison officers, Aboriginal health service and the members of the newly established Indigenous Reference Groups (IRG) from the region. These materials were utilised during the small group formal education and informal yarning sessions during the Transplant Outreach Clinics. Work is ongoing to create flip-books and posters. Indigenous Reference Groups were formed across the Kimberley region. Three multi-disciplinary Outreach Clinics were conducted in the region, attended by transplant physicians, surgeons and nurses. This resulted in an increase in the number of Aboriginal patients undergoing assessment from 10 to 71, with 23 being approved for transplant suitability. Several patients were identified to have modifiable barriers to transplant work-up. The number of patients active on the transplant waitlist increased from 4 to 12 within a year of outreach visits. To date, 6 patients from the region have successfully received a transplant. Feedback from patients has been overwhelmingly positive.
Conclusion: Improving access to KTx and transplant outcomes for Aboriginal Australians requires a collaborative, holistic and culturally safe approach to the delivery of care. At the core of addressing the inequality in access to kidney transplantation, is the need to effectively communicate, engage and empower the Aboriginal patients and their communities.
National Indigenous Kidney Transplantation Taskforce Equity & Access Sponsorships, Australia.

right-click to download
