
Antibody response and cellular phenotyping in kidney transplant recipients following SARS-CoV-2 vaccination
Nicole Ali1, Zoe Stewart1, Jake Miles2, Sapna Mehta1, Vasishta Tatapudi1, Bonnie Lonze1, Elaina Weldon1, Charles Dimaggio1, S Gray-Gaillard1, Jeanette Leonard1, S Tuen1, Robert Montgomery1, Herati Ramin1.
1Transplant Institute, NYU Langone Health, New York, NY, United States; 2CareDx, CareDx, Brisbane, CA, United States
Introduction: Correlates of protection for SARS-CoV-2 vaccines are not yet well-established in kidney transplant recipients (KTRs). Studies have highlighted the importance of neutralizing antibodies (Abs), however data suggests T cell responses may play a secondary role in preventing reinfection. We performed a longitudinal assessment of immunogenicity and T and B cell responses in KTRs following SARS-CoV-2 vaccination.
Methods: KTRs eligible for SARS-CoV-2 vaccination were screened through medical records from March 12, 2021. Baseline and weekly blood samples were collected for routine assessment, SARS-CoV-2 spike protein Ab titers and cellular phenotyping for 12 weeks. Ab response was defined as a 10-fold increase in total binding IgG titers. To determine if T cell responses were induced by vaccination, we considered the proportion of activated non-naive CD4+ and CD8+ T cells after vaccination.
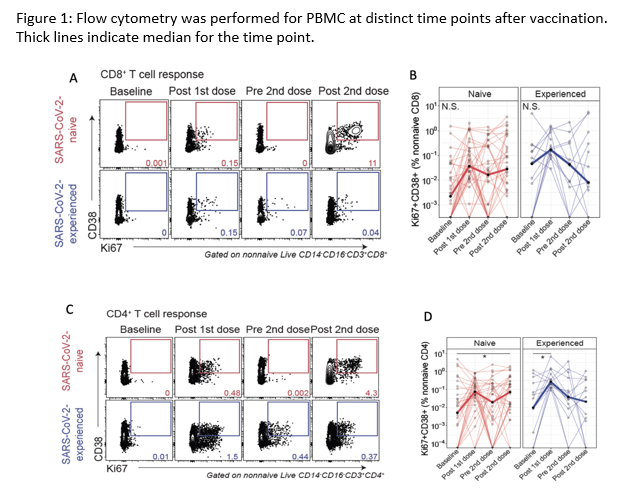
Results: 49 KTRs with a mean age of 54 years were enrolled (Table 1). 10 patients (20.4%) mounted an Ab response following completed vaccination. A history of COVID-19 was associated with an increased likelihood of developing an Ab response (OR: 18.3, 95% CI 3.2, 105.0, p=0.0005). For non-naive CD8+ T cells, a subset co-expressing CD38+Ki67+ was induced 1 week after the 1st immunization in some SARS-CoV-2-naiive patients (P=0.12 versus P=0.14 for SARS-CoV-2-experienced adults, Figure 1A/B). For non-naive CD4+ T cells, induction of a subset co-expressing CD38+Ki67+ was observed at 1 week after the 1st immunization for SARS-CoV-2-naïve participants (P = 0.09 for SARS-CoV-2-naïve, P=0.03 for SARS-CoV-2-experienced adults, Figure 1C/D). For CD8+ and CD4+ T cells, dose 2 stimulated weak induction of the CD38+Ki67+ subset in the SARS-CoV-2-naïve patients only (Figure 1A-D).
Conclusions: Quantitative Ab responses were strongly associated with prior SARS-CoV-2 infection. Activated CD4+ and CD8+ T cell responses were evident in most patients, with wide variation, irrespective of COVID-19 history. Further studies are needed to determine whether these activated CD4+ and CD8+ T cell responses were antigen-specific or confer immunity.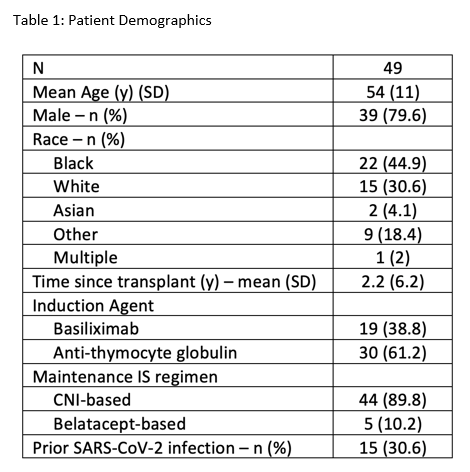

right-click to download
