C-reactive protein and urea levels distinguish primary non-function from early allograft dysfunction after liver transplantation
James Halle-Smith1, Lewis Hall1, Angus Hann1, Keith Roberts1, Hermien Hartog1, Thamara Perera1.
1Liver unit, Queen Elizabeth Hospital Birmingham, Birmingham , United Kingdom
Introduction: A spectrum of graft dysfunction occurs after liver transplantation (LT), ranging from early allograft dysfunction (EAD) to primary non-function (PNF). There are no single or uniformly accepted laboratory parameters that differentiate these entities. Several biochemical markers are exclusively made in the liver, including urea, C-reactive protein (CRP) and fibrinogen. However, these are given les prominence than transaminases, bilirubin and International Normalised Ratio (INR). The aim of this study was to determine if routinely measured serum biochemical markers can distinguish PNFfrom EAD in the initial 48 hours following deceased donor liver transplantation.
Methods: A retrospective study of all adult patients that underwent LTat our institution between January 2010 and April 2020 was performed. Patients that experienced graft loss from a complication other than PNF in the initial 14 days were excluded. Patients were grouped into an immediate graft function (IGF), EAD, and a PNF groups. The absolute values and trends of CRP, blood urea, serum transaminases, INR and fibrinogen in the initial post-operative 48 hours were compared between groups. Biochemical factors found to be significantly different between groups on univariable analysis were further investigated using receiver operating characteristic (ROC) curves. The area under the receiver operating characteristic curve (AUROC) value was reported, and the Youden index was used to identify the optimum cut-off values.
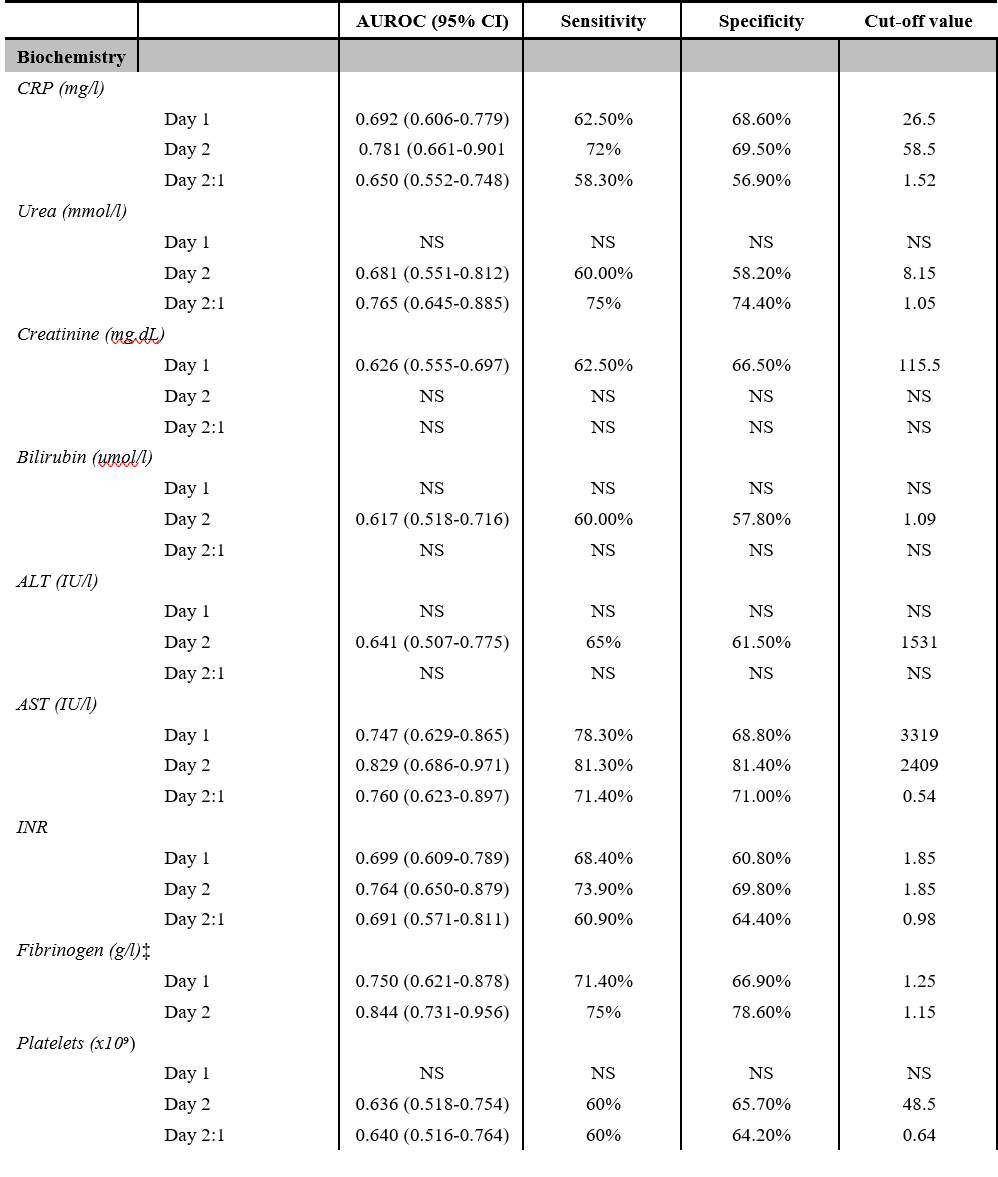
Results: During the study period, 2102 LTs were performed and 1937 were eligible for inclusion. There were 1394 patients with IGF (72%), 503 with EAD (26%) and 40 with PNF (2%) patients according to the study definition. A significantly greater proportion of grafts were from donors following cardiac death (DCD) in the PNF group compared to the EAD group (45% vs. 29%; p=0.04). The median (IQR) of each variable and the accuracy in distinguishing PNF from EAD is demonstrated in table 1 and 2 respectively. Lack of an increment in CRP (Day 2:1; 1.43 v 1.77, P=0.01) and urea production between on day 1 and 2 ( Day 2:1; 0.71 vs 1.32, P=<0.01). The CRP level was significantly lower in the group that experienced PNF on both day 1 and 2 (Day 1; 20 v 43, P=<0.01, Day 2: 24 v 47, p=<0.01,). Urea production was significantly lower on post-operative day 2 in the PNF group (Day 2; 5.1 v 9.0, p=<0.01). An aspartate transaminase (AST) threshold of 2409 IU/L on post operative day 2 had the highest accuracy in distinguishing PNF from EAD (AUC; 0.83, Sensitivity: 81.3%, Specificity 81.4%). 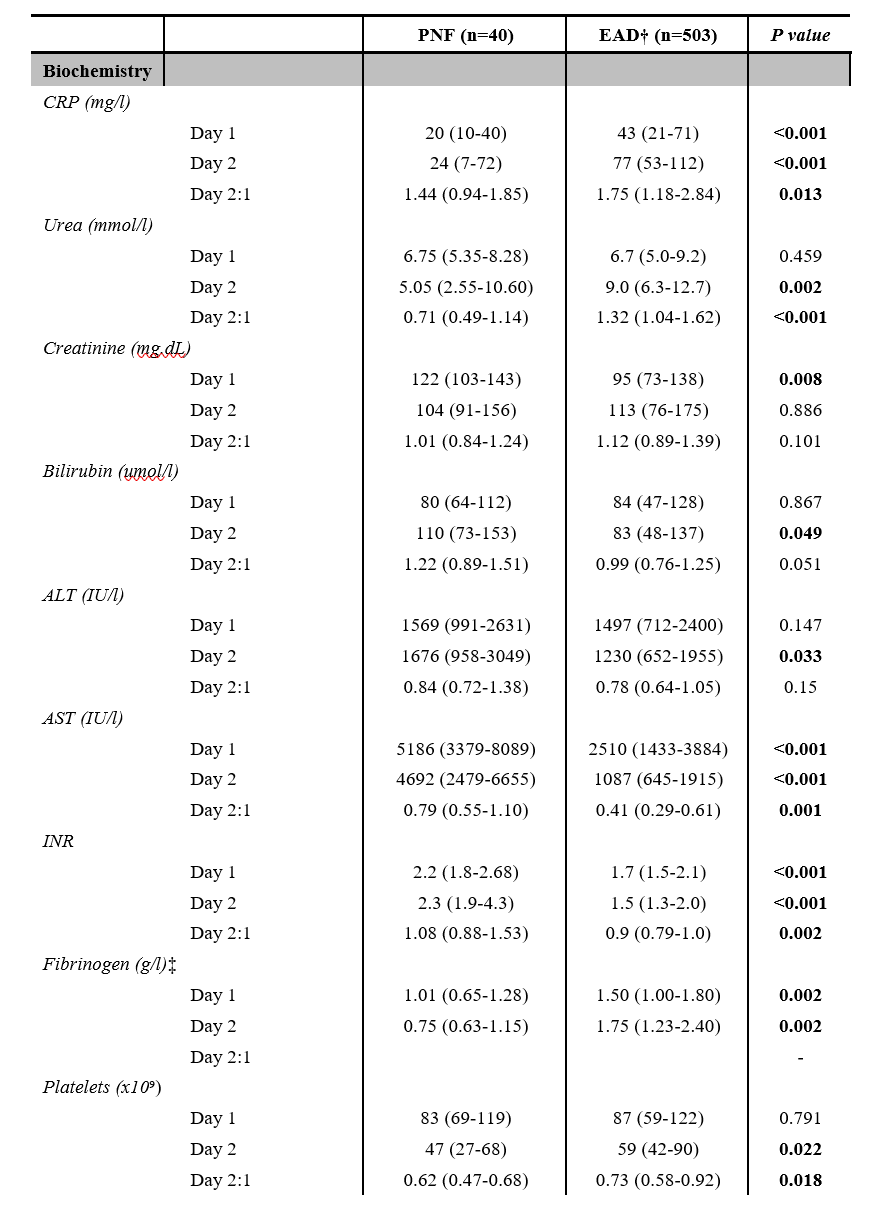
Discussion: CRP and AST are more effective than ALT and bilirubin in distinguishing PNF from EAD in the initial post operative 48 hours. Clinicians should consider the values of these markers when making treatment decisions for patients with early liver allograft dysfunction.

right-click to download
