
Guang-Peng Zhou, PhD
Liver Transplantation Center, National Clinical Research Center for Digestive Diseases, Beijing Friendship Hospital, Capital Medical University; Clinical Center for Pediatric Liver Transplantation, Capital Medical University, Beijing, China. Email: guangpeng_zhou@ccmu.edu.cn
Dr. Guang-Peng Zhou is now a clinical postdoctoral fellow and a resident at the Liver Transplantation Center of Beijing Friendship Hospital, Capital Medical University. Since 2015, he has been under the tutelage of Professor Zhi-Jun Zhu, a famous liver transplant surgeon in mainland China, and has participated in over 100 cases of liver transplantation, including living donor liver transplantation and auxiliary liver transplantation. Under the leadership of Professor Zhi-Jun Zhu, their team completed the first case of cross-auxiliary double domino donor liver transplantation in 2013 and the first case of cross-auxiliary domino liver transplantation by exchange of partial liver between two patients with hypermethioninemia and OTCD in 2018. "Liver transplantation without donation" can be achieved by this way. He is currently engaged in clinical and basic research related to liver transplantation and hepatocyte transplantation for the treatment of inherited metabolic liver diseases. He has published several scientific research papers in international journals as the first or co-first author and participated in international conferences including IPTA and ILTS as oral or poster abstract presenter for several times. He obtained “Young Investigator Awards” in 2022 Joint International Congress of ILTS, ELITA, & LICAGE.
No difference in posttransplant survival among patients with or without nonalcoholic steatohepatitis: a meta-analysis and meta-regression
Guang-Peng Zhou1,3, Yi-Zhou Jiang1,2,3, Li-Ying Sun1,2,3, Zhi-Jun Zhu1,3.
1Liver Transplantation Center, National Clinical Research Center for Digestive Diseases, Beijing Friendship Hospital, Capital Medical University, Beijing, People's Republic of China; 2Department of Critical Liver Diseases, Liver Research Center, Beijing Friendship Hospital, Capital Medical University, Beijing, People's Republic of China; 3Clinical Center for Pediatric Liver Transplantation, Capital Medical University, Beijing, People's Republic of China
Background & Aims: Nonalcoholic steatohepatitis (NASH) is a dramatically growing indication for liver transplantation (LT) worldwide. The posttransplant outcomes of NASH patients are currently under intensive investigation. Given the enormous volume of new studies with inconsistent results, we conducted a meta-analysis aimed to update the clinical evidence on the long-term outcomes of transplanted patients with NASH.
Methods: We comprehensively searched MEDLINE, Embase, Cochrane Library, and Web of Science databases through September 15, 2021, for comparative studies focusing on outcomes of LT recipients with NASH and indications other than NASH. Random-effects meta-analysis was conducted to calculate pooled odds ratios (ORs) and 95% confidence intervals (CIs). Meta-regression was used to examine hepatocellular carcinoma (HCC) as a confounder on patient survival.
Results: Twenty-two studies with 1,538 NASH and 6,014 non-NASH patients were included. 1- (OR, 0.94; 95% CI, 0.77–1.14), 3- (OR, 0.82; 95% CI, 1.00–1.22), and 5- (OR, 1.05; 95% CI, 0.84–1.31) year patient survival was equivalent between NASH and non-NASH recipients. 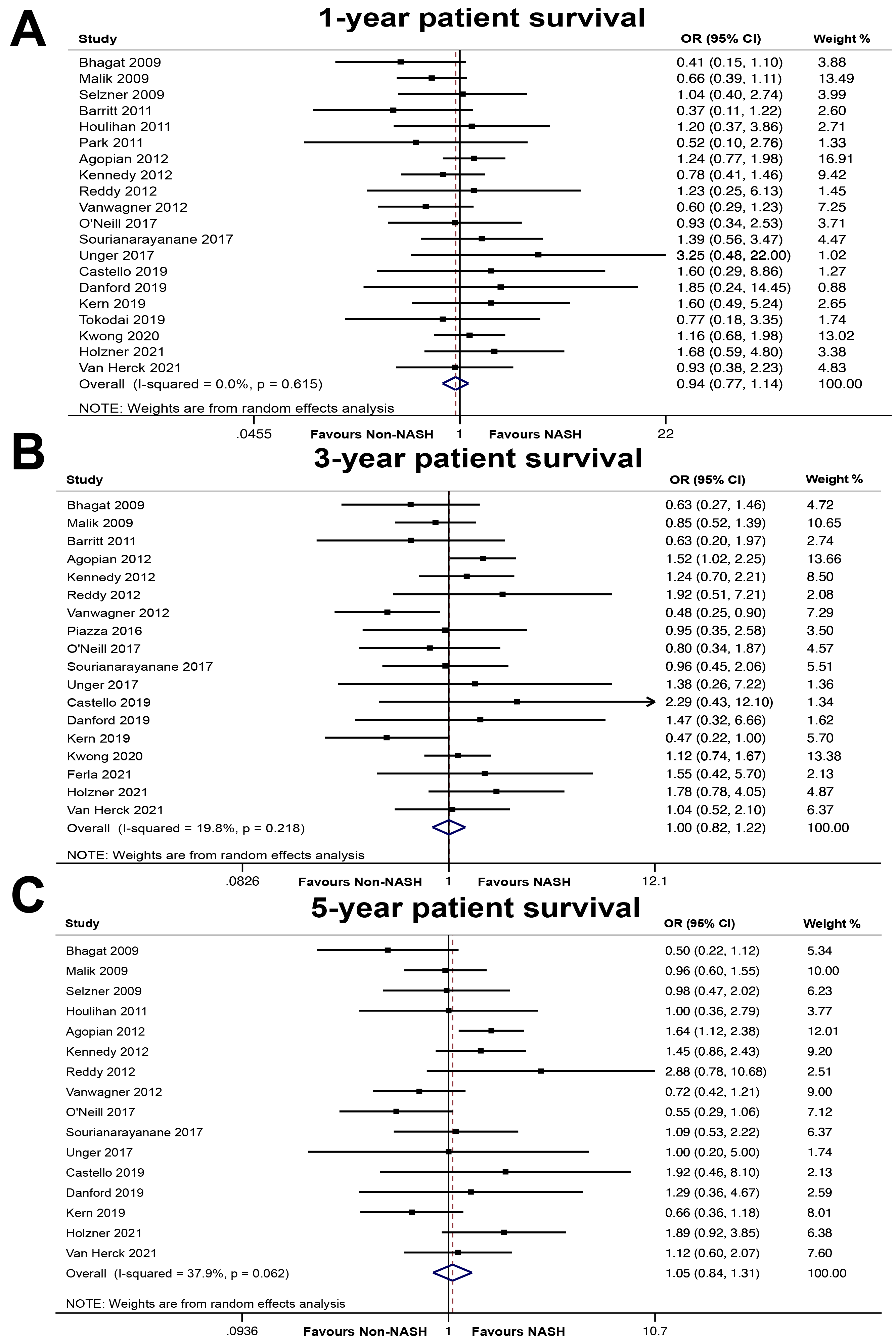
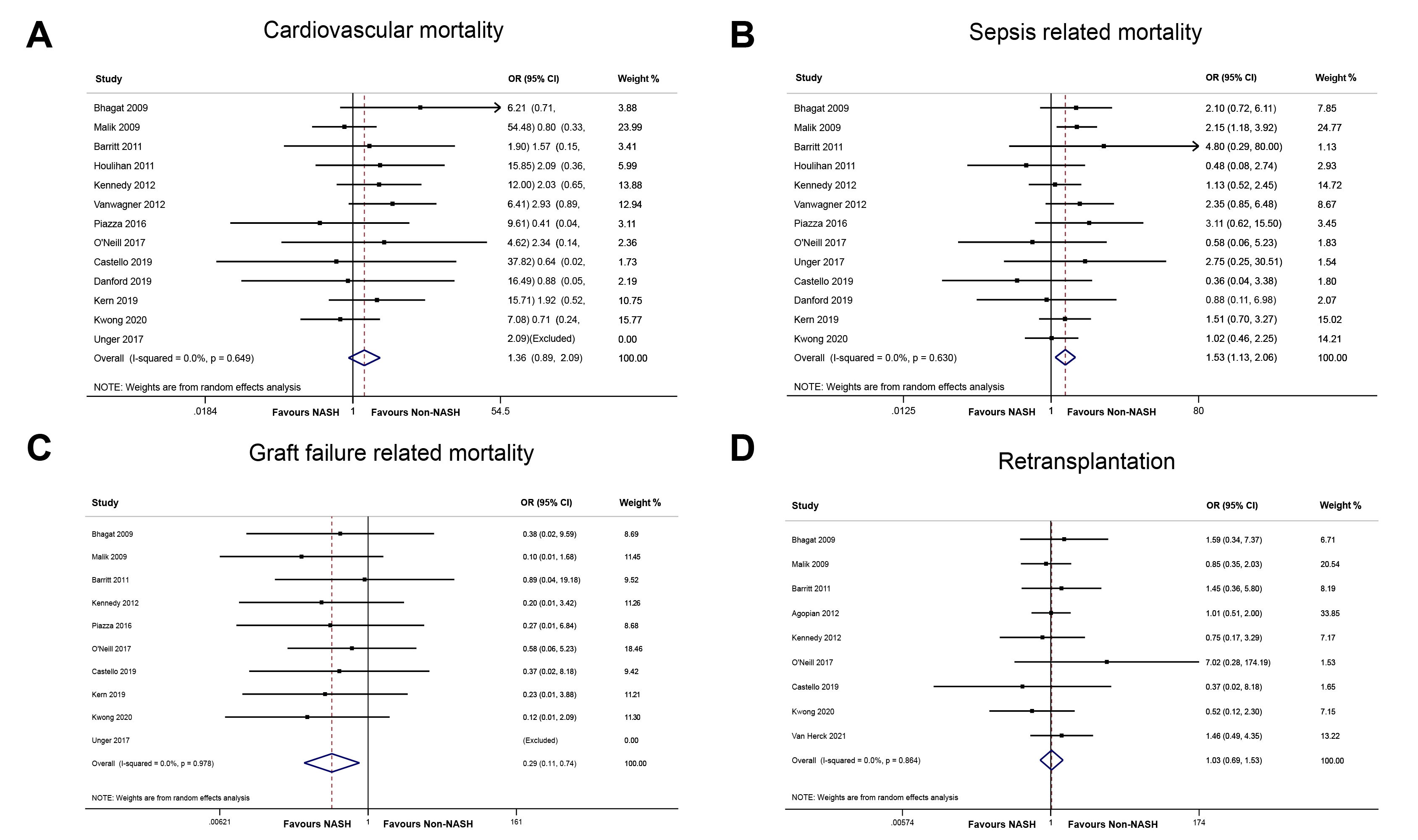
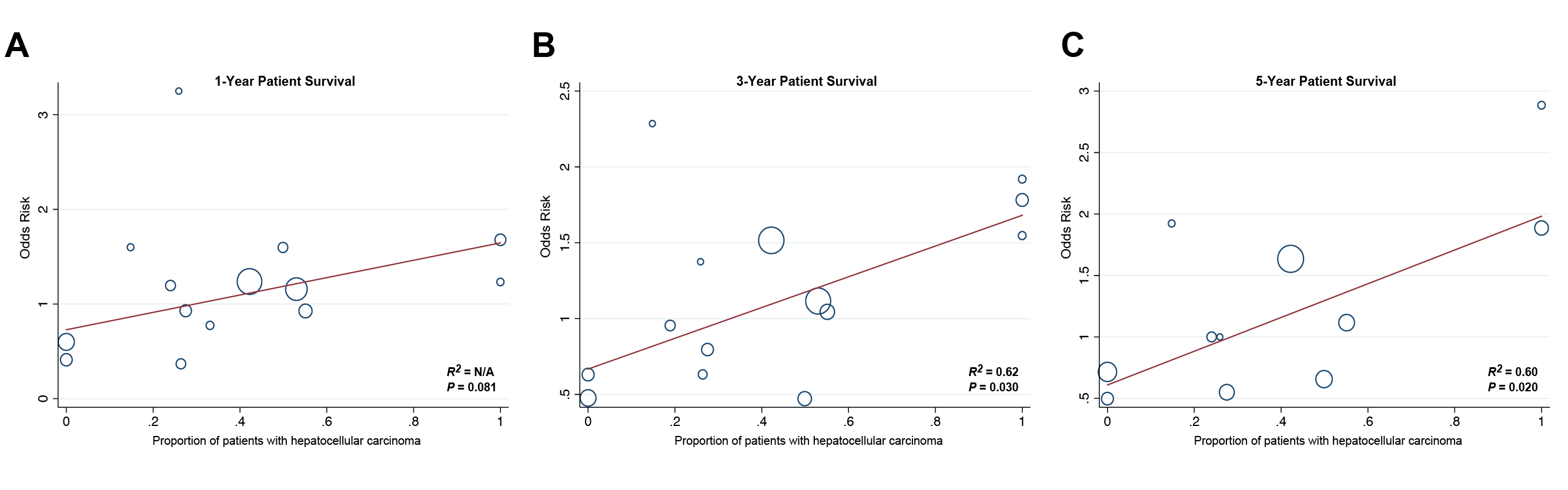
NASH patients were associated with similar cardiovascular mortality (OR, 1.36; 95% CI, 0.89–2.09) and retransplantation rates (OR, 0.69; 95% CI, 1.03–1.53), lower graft failure-related mortality (OR, 0.11; 95% CI, 0.29–0.74), but higher sepsis-related mortality (OR, 1.53; 95% CI, 1.13–2.06). In meta-regression analysis, the proportion with HCC showed a strong correlation with posttransplant survival.
Conclusions: This pooled analysis of a large global sample size showed no difference in posttransplant survival between NASH and non-NASH patients. NASH recipients should be managed with caution after LT, especially regarding the potentially high risk of sepsis-related death.

right-click to download
